While it should not be common, a complication that you will see on more than one occasion in All-On-X surgery, is incision line dehiscence.
A dehiscence can be troublesome as it can create the following:
- Increased infection risk.
- Pain and discomfort for the patient.
- Poor tissue healing around implants and abutments.
- The creation of bony sequestra, causing bone loss at an implant site.
We have previously discussed how to treat an acute post op wound dehiscence.
But why does a dehiscence happen in the first place and how can we prevent it?
Listed below are 10 reasons why an AOX incision might dehisce. Just as important, are suggestions as to how we might avoid this scenario altogether.
10 Reasons Why an AOX Incision Dehisces
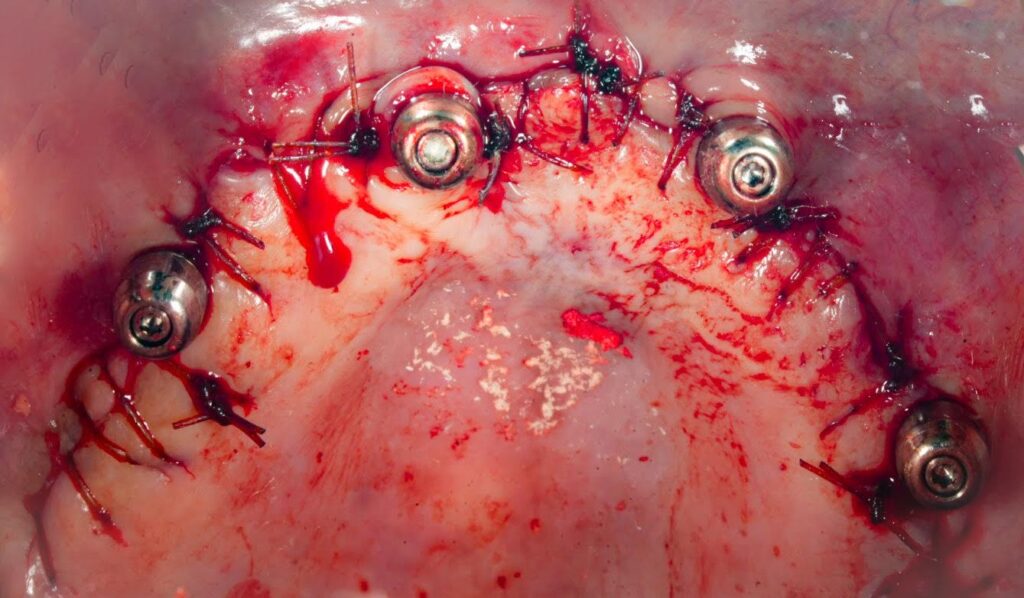
1. One single, continuous suture per arch.
While this is a popular technique, I am not a fan of a single continuous suture for one principle reason:
If any part of your suture comes undone or loosens, you can have your whole arch incision dehisce.
I prefer to run a separate suture between adjacent implant sites, with the addition of an occasional interrupted suture if extra support is indicated. Therefore I place 5 individual, short, continuous sutures per arch. If one does come undone, I’ve got a much smaller dehiscence to manage.
2. A suture that resorbs too quickly.
Given that this is a full arch incision and not a single tooth extraction site, we need to use a suture that will hold the wound closed long enough for primary healing to occur.
Plain gut suture, in my experience, resorbs too quickly. This is inadequate for holding a large AOX incision together long enough for optimal healing.
Vicryl suture is more than adequate in its duration of action. And many practitioners opt for this suture as their go-to. In my practice, I notice that Vicryl actually lasts too long, and patients complain about its tissue irritation.
Non-resorbable sutures are not a wise choice as removing them underneath the prosthetic at a post-op is next to impossible, not to mention unpleasant for patients that tend to be prone to dental phobias.
I find the best suture for most AOX cases is a chromic gut suture. Its duration of action is long enough to hold the wound closed in the majority of cases, but short enough to resorb before patients notice significant tissue irritation.

3. Waterpik use immediately post-op.
Many patients, despite the post-op instructions they were given, begin waterpik use right after surgery in an effort to keep their new teeth clean.
The force of the waterpik applied to the fresh incision line will almost always blow the wound open. And, if miraculously it does not, it will dissolve the sutures too quickly allowing the wound to dehisce over time.
It is very important to ensure that patients do no more than a gentle Chlorhexidine and/or salt water rinse/monoject irrigation, until tissue healing is confirmed at their follow up. Once adequate soft tissue healing is confirmed, they can then begin waterpik use at that time.
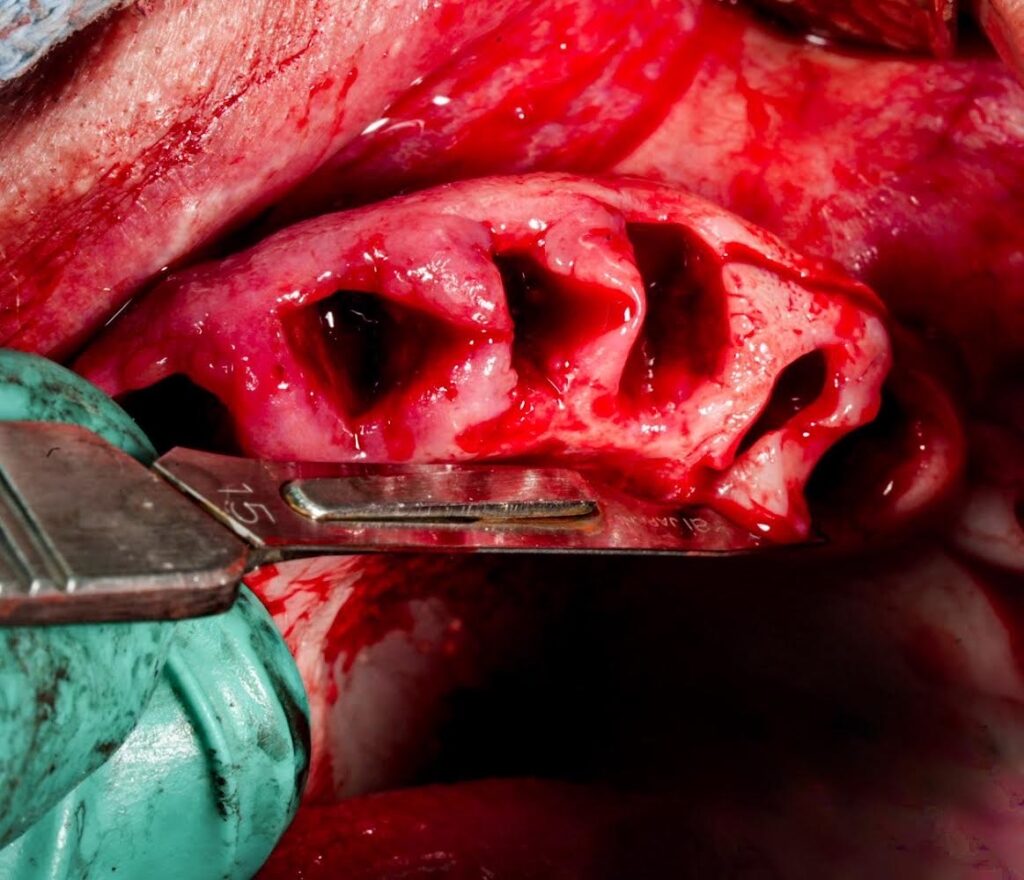
4. Inadequate removal of granulomatous, inflamed, periodontally involved tissue.
Many AOX patients will present with extensive periodontal disease and inflamed, granulomatous attached tissue.
If this tissue is not removed prior to closure the following can happen:
When suturing, the edematous, inflamed tissue is much more likely to put tension on the wound – pulling the wound apart.
Granulomatous tissue is also more likely to have the suture mechanically “pull through” during the healing period as the tissue is not as strong as healthy gingiva.
This creates a much higher likelihood a wound dehiscence will occur in this area.
I always attempt to remove all granulomatous, inflamed, periodontally involved tissue prior to closure.
Yes, this can be a fine line with trying to preserve keratinzed tissue. But at the end of the day, I want healthy, non-periodontally involved tissue wrapped around my implant – even if that means a little less keratinized tissue.

5. Extensive post-op swelling and edema, creating increased wound tension.
Intraoral and facial swelling is par for the course with AOX surgery.
Furthermore, every patient is unique. Some patients will swell and bruise more than others. For some patients, it’s hard to tell they even had surgery at all.
That being said, excessive soft tissue swelling can create increased wound tension that will pull at your incision line, and can cause the soft tissue to actually tear through the sutures and dehisce.
Being cognizant of surgical technique and efficiency is critical to help minimize post-op swelling and limit the chance of wound dehiscence.
6. Poor healing due to an immune compromised state.
I treat many AOX patients who present with multiple medical comorbidities. Of these, I commonly see diabetes and autoimmune disorders.
While these medical diagnosis are not necessarily a contraindication to treatment, they can affect both soft and hard tissue healing.
Unfortunately, I cannot remove every risk of infection or poor healing in any patient, let alone immune compromised patients.
What I can do though, is work with these patients’ physicians pre-operatively to ensure they are medically optimized prior to surgery. This will give them their best chance of successful wound healing and limit the chance of acute post-op issues such as a wound dehiscence.
7. Your referring doctor removes a suture to adjust and/or access an abutment during the pick-up, but does not realize it is a running suture…
While this may sound odd and unlikely to happen to you… this has happened to me.
In an effort to more easily access an abutment immediately post-op, my referring doctor cut what they thought was one suture. However they did not realize it was a running suture between those two implants. Needless to say the suture in this area did not fair well.
Since then, I have made it clear to my referring doctors that if there is ever a need to remove a suture to please inform me prior. This way, I can help navigate and instruct how best to manage the situation.
8. Removal of too much soft tissue prior to closing the incision.
I always remove the interdental papilla and attempt to create a smooth straight tissue margin on all aspects of my incision for an even, flat closure.
I have a lot of practice at this technique now, but when I first started there was more than one instance where I removed slightly too much tissue. Although I was still able to achieve primary closure in these instances, I had to pull and stretch the tissue to achieve that closure.
Removing too much tissue prior to closure creates this need to pull the wound closed. This produces extra tension and leads to an increased risk of wound dehiscence.
Proper incision design and closure technique should be well thought out and practiced to ensure enough tissue is left to close, but that there is also not an excess of tissue that has difficulty laying flat and smooth.
9. Overuse of Cautery
While this is anecdotal, I have noted among colleagues an increased incidence of dehiscence when extensive electrocautery is used both for soft and hard tissue management.
I must say that I do know some surgeons who use electrocautery frequently, but strategically, and do not have this issue.
That being said, I very, very rarely use electrocautery.
The only time I use it is to help stop a significant bleed.
I do not like the idea of any desiccation or cauterization of any soft or hard tissue around my implant sites.
We work so hard to prevent overheating of our bony osteotomies, that it makes no sense to me to perform electrocautery on or adjacent these sites.
I want healthy, clean, bleeding margins for both the hard and soft tissues around my implant sites.
In my opinion, in regards to cautery… less is more.
10. Engaging an inadequate amount of tissue during closure.
While this may sound obvious, it can happen to all of us. Engaging an inadequate amount of tissue with your suture needle on either side of the incision line, can cause the suture to pull through the tissue when under tension.
Remember that tension will increase as swelling increases in the post-op period.
Placing your suture needle ~2-3mm away from the incision line will normally provide enough tissue strength without “balling up” the tissue with too big of a “bite”.
If you do enough All-On-X surgery, you will have wound dehiscences occur. It is simply part of surgery.
That being said, it should not be a common occurrence. If you notice your incision line dehiscing on a recurring basis, take a look at the items listed above and see if one of the simple adjustments suggested can help you avoid this post-op complication.
Here’s to our incisions… sticking together when times get tough.
Matthew Krieger DMD

Pingback: To Remove, Or Not to Remove: That is the Question. - AOX Surgery