Archived Newsletter Re-Post.
The AOX Newsletter • January 2024 #1
My target torque value for all of my implants is 45-60 N-cm. You can read more about why here.
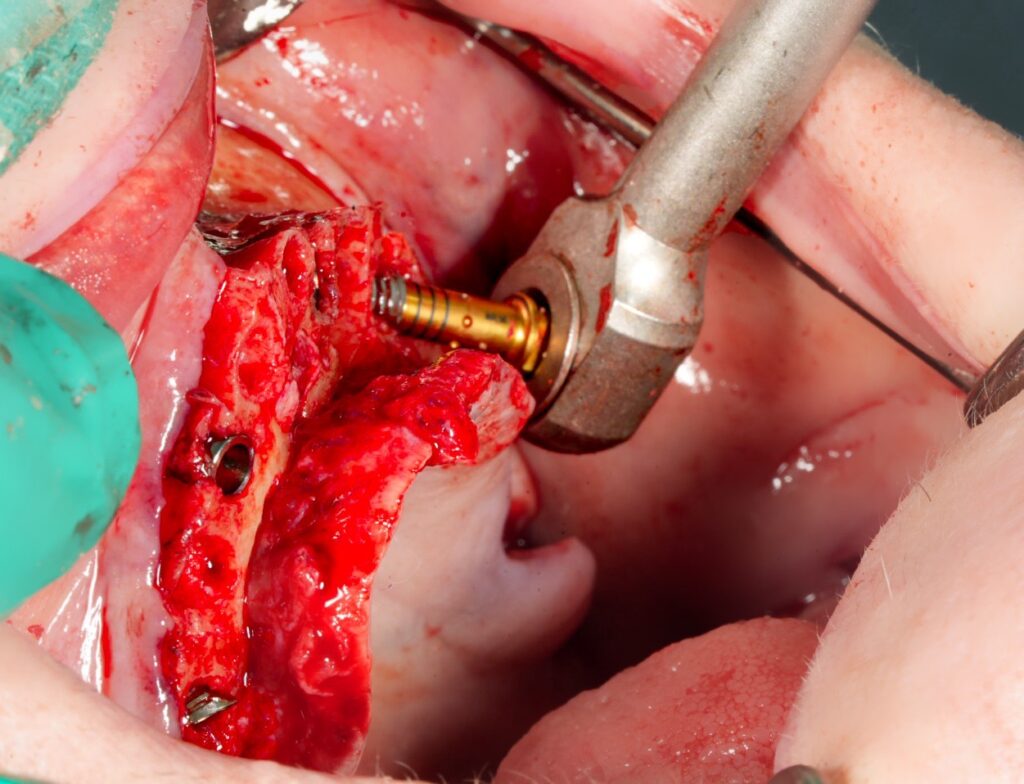
In order to fully seat my implants and to confirm the torque value, I utilize a torque wrench with a torque gauge. The torque wrench I use has a gauge that indicates torque up to 60 N-cm. Beyond that it’s an estimated guess.
My handpiece will torque out at right around 60 N-cm, with the implant often situated slightly above the alveolar crest. I then insert my torque wrench and immediately attempt to turn the gauge to 60 N-cm. If I am able to do this – that’s it. I’m done checking torque. I ratchet the implant the rest of the way down and call it a day with a torque of 60+ N-cm.
If I check the torque and the implant rotates prior to 60 N-cm, I then move forward without hesitation, efficiently ratcheting the implant all they way to the desired final position – without checking the torque in between. On my FINAL turn, I check the torque at this point and record that value.
One large efficiency mistake I see many new providers make is checking their torque value every… single… time… they… turn… the… torque… wrench. Many even pause for a few seconds to look at the torque value each time. This can mean 4…7… 9… or even 11 turns and checks of the torque wrench!?
Why!?? All you need to know is: Is it 60 N-cm or above (or whatever your highest gauge reading is)? If not, what is the FINAL torque value?
At most, we should all be checking our torque twice. And more often than not, once is all that is required.
And then – move on.
Cheers to efficiency,
Matthew Krieger DMD
“Don’t equate activity with efficiency.”
Harvey Mackay
Q & A with Dr. K

“What is your post-op follow up schedule?”My patients return 24 hours after surgery for assessment and delivery of their prosthesis by the prosthodontist. Patients are then seen for a post-op follow up at 10-14 days. If I have any specific concerns that I feel warrant further attention, I will see patients back again at the 3 week mark. Should healing continue on a routine course, patients are then seen at 4 months to confirm osseointegration. |
Archived newsletters are released on a delayed timeline, a few months after the original publication. If you would like to receive these newsletters in real time please sign up here.

thank you for the information sharing ,
how you confirm osseointegration, do you use ISQ measuring device
There are a lot of fancy tools and techniques to confirm osseointegration. However, in my experience, integration at a 4 month follow up in AOX surgery is usually very obvious.
I look for:
1. The presence or absence of “Subjective Symptoms” (patient should not be having pain at implant site)
2. The presence or absence of of “Clinical Signs” of infection (ie. swelling, purulence, tenderness, mobility).
3. The presence or absence of “Implant Stability” (if an implant is not integrated it will be loose…this should be very easy to tell even with manual digital pressure on the abutment. But, you can also perform a torque test of the implant if you are unsure).
That’s honestly really all that I do…
If for some reason I am uncertain, I will also perform a percussion test on the implant/abutment but this is not something I normally do.
If an implant hasn’t integrated…it’s usually loose, painful and quite obvious.