The beloved Midline Implant.
A favorite of many a practitioner and part of the 5 Implant Configuration used frequently in All-On-X surgery.
As someone who almost never…ever…places a midline implant, I have struggled to grasp the value in this technique.
Furthermore, I think the midline implant can actually be a disadvantage to your AOX cases, your patients, and your practice.
I realize that’s a very controversial statement.
But, let me explain below why I feel this way and subsequently why I almost never…ever…utilize this technique.
7 Reasons Why I Almost Never…Ever…Place a Midline Implant
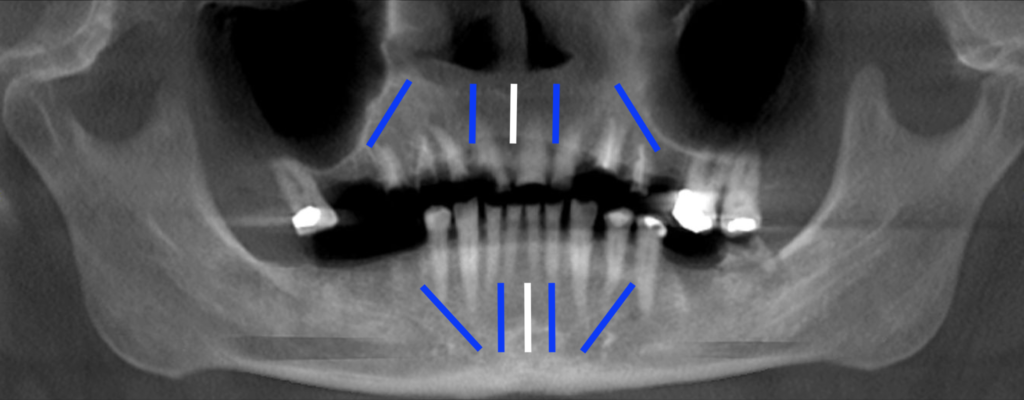
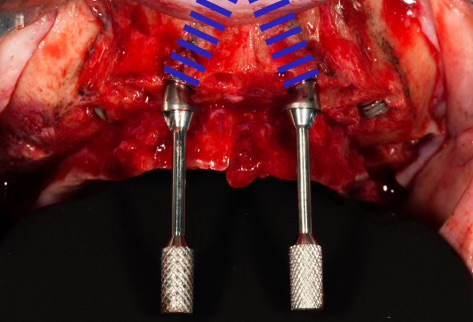
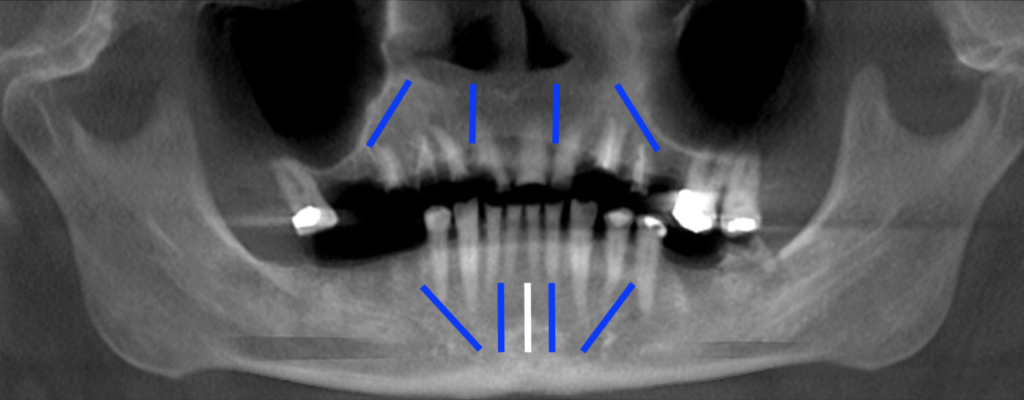
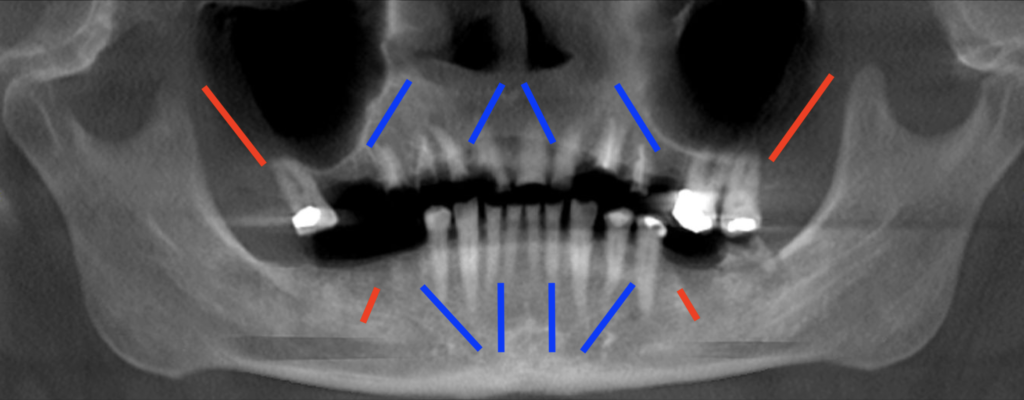
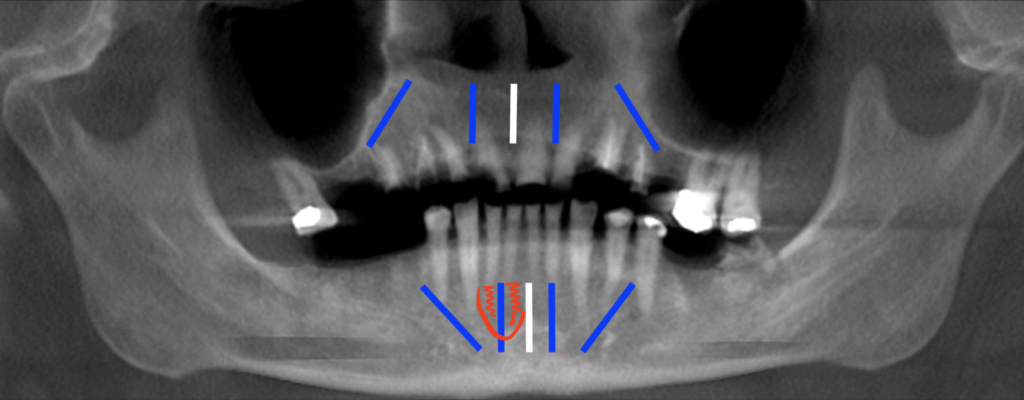
1. A midline implant prevents utilization of the Maxillary Inverted V Configuration.
I am absolutely convinced that the Inverted V Configuration is the best way to place your anterior maxillary implants.
Unfortunately, placement of a midline implant prevents the use of the Inverted V Configuration. You cannot angle your lateral incisor implants toward the midline, because there is already an implant in this location.
With its presence, the midline implant voids all the benefits of the Inverted V Configuration. This includes improved torque, increased implant length, and preserving bone real estate should you need to remove and replace an implant in the future.
The fact that a midline implant prevents the Inverted V Configuration is enough to make me never want to place one again.
But this is just the tip of the iceberg…
2. A midline implant is actually NOT a great “back-up” implant…
I have heard many times from practitioners that they place a midline implant because:
“It provides a back-up implant. If an implant fails I don’t have to replace it”.
Ok…
Let’s delve into this a little deeper.
In reality, the only implant you do not need to consistently replace if it fails…is the midline implant. Every other implant will likely require replacement should it fail.
If a posterior implant at site #4 or #13 fails…you better believe you will need to replace it. You must maintain adequate posterior support for your prosthetic and prevent an excessively long cantilever. Unfortunately, the midline implant is of absolutely no help in this scenario.
Ok, well what if #7/10 fail? Your midline implant should surely save the day in this scenario correct?
Not necessarily.
If adequate A-P spread was achieved, there is a very strong possibility your posterior implant will be a notable distance in the arch form from your midline implant.
This distance can often be 30mm or greater. In an acrylic prosthetic, this will create a weak point prone to fracture and can compromise the integrity of the prosthetic.
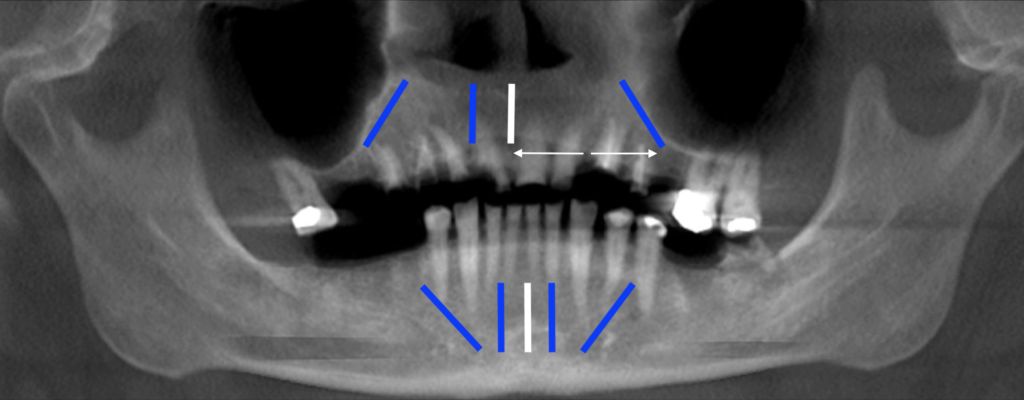
In this scenario the ideal treatment would be to replace the lateral incisor implant to avoid creating a fracture point in the prosthetic.
If you are in a final prosthetic, you may be able to get away with this span between implants. However, the point is simply that having a midline implant does not always mean you do not have to replace a failed lateral incisor site.
So, finally, what if your midline implant fails?
Well, don’t stress too much. You almost certainly don’t need to replace it. Why? Aside from some very rare circumstances, it wasn’t necessary to begin with.
3. A midline implant is a very expensive technique that does not make financial sense.
I have heard the following argument in favor of the midline implant on more than one occasion:
“I don’t want to pay to remake a prosthetic if an anterior implant fails”.
The thought process is that by adding the extra midline implant, should an anterior implant fail, you can just remove the failed implant and utilize the remaining two anterior implants. In this scenario you would not need to add an additional implant and/or remake the prosthetic. The patient simply continues to wear their existing prosthetic.
As I’ve outline above, unfortunately the presence of a midline implant does NOT always mean you do not need to replace a failed anterior implant.
But…if we were to theoretically assume that was the case (which it’s not)…Let’s look at the financial math behind this strategy.
Cost Analysis of a Midline Implant
The prosthetic cost is going to vary greatly depending on if the patient is in a temporary acrylic prosthetic or a final prosthetic at the time of failure. It is also going to vary depending on if the restorative provider is utilizing an outside lab or printing/milling their own prosthetics. Furthermore, it will depend on the quality of the lab and final material chosen.
I’m going to be generous and help out those in favor of the midline implant. Let’s assume that your patient was already in a final prosthetic and you are using an outside lab….
Cost to Remake Final Prosthetic: $2500
Now, looking at the surgical aspect, a good goal should be an implant failure rate of ~2% with All-On-X surgery.
Therefore out of 100 arches (500 implants with the midline implant), we can assume a failure of 10 implants.
Let’s assume a fairly even failure distribution. In this case, of those 10 failures 5 are posterior implant sites and 5 are anterior implant sites.
This means we have 5 unique anterior implant failures and therefore 5 affected arches. IF we are buying into the argument that these do not need to be replaced since a midline implant is present, and therefore the arch does not need to be remade….we have just saved ourself the expense of remaking 5 arches.
Cost Savings as a Result of Not Remaking 5 Arches = 5 Arches x $2500/Arch = $12,500
Ok…saving $12,500 per 100 arches is great.
But let’s also look at our expenses to provide that midline implant….which theoretically prevented us from having to remake those 5 arches.
Just like the prosthetic, implant costs can vary greatly. Implant out of pocket costs to doctors can range from $150 up to $600 depending on the style, brand, and your practice volume. For the sake of this article, I am going to calculate a reasonable “average” cost of $300/implant.
Expenses Related to Midline Implant Placement = 100 Arches x $300/100 Midline Implants = $30,000
In this scenario you have spent $30,000 in order to save $12,500 🧐.
Not to mention you have donated your time for 100, arguably unnecessary implants.
While this math will vary with different practices, outside of some extraneous circumstances, the take home message remains the same: A midline implant is simply not a cost effective method of treatment.
4. A midline implant is not the best way to improve A-P spread.
Many proponents of the midline implant feel that it improves A-P spread by extending implant placement further anterior and therefore assisting with elimination of a facial cantilever.
In theory, this can be true depending on your implant placement configuration and could be a potential indication for a midline implant.
However, this is only plausible if your anterior implants at #7/10 are either placed distal to the #7/10 sites toward the canine region, and/or if your implants at #7/10 are placed too far palatally for a less than ideal prosthetic screw access.
In these scenarios…you can argue that a midline implant is beneficial.
And…I would agree.
However, my proposal is the following:
Why not place anterior implants #7/10 in a more favorable prosthetic position in the first place? It’s less surgery, less overhead, and solves the problem of the facial cantilever and/or poor anterior extension of the A-P spread.
If the anterior implants are placed in a close to ideal position, a midline implant will not actually accomplish any notable improvement in A-P spread and/or elimination of a facial cantilever.

5. More than 4 Implants is NOT always better.
As surgeons we have a tendency to want to always place more implants.
Many practitioners that use the midline technique have told me that,
“More than 4 implants is always better when you can do it”.
While our literature is ever-evolving and always changing, to my knowledge evidence based practice has not yet found a significant difference between surgical and prosthetic AOX success rates and the use of “more than 4 implants”.
Polido et al. concluded:
…the use of fewer than five implants per arch, when compared to five or more implants per arch, to support a fixed prosthesis of the completely edentulous maxilla or mandible, present similar survival rates, with no statistical significant difference…
While I do subscribe to this philosophy, one variable that is always on my mind is cantilever length. I do attempt to eliminate or minimize the cantilever in each AOX surgery. However, with this goal in mind, I tend to almost always place either 4 implants…or 6 implants.
A 6 implant configuration, when indicated, allows me to eliminate a cantilever bilaterally. A midline 5 implant configuration offers me no such benefit. So even when I do actually feel “more is better”, I am looking to go to a 6 implant design, not a midline 5 implant configuration.
6. There are better ways to improve composite torque than a midline implant.
A midline implant will technically improve composite torque. But, is this actually the best way to go about improving composite torque in a low density, immediately loaded case?
In my opinion it is not.
In cases where I encounter truly low density bone and am struggling to reach a loadable composite torque value of 120 N-cm, the last thing on my mind is a midline implant.
Why?
If I have a low density, low torque case, I want to accomplish two goals: I want to increase my torque value AND eliminate any cantilever. I do not want to load a low composite torque case AND leave a cantilever.
Therefore, in these scenarios I am always attempting to transition to a 6 implant configuration in order to accomplish both an increased composite torque value and elimination of the cantilever.
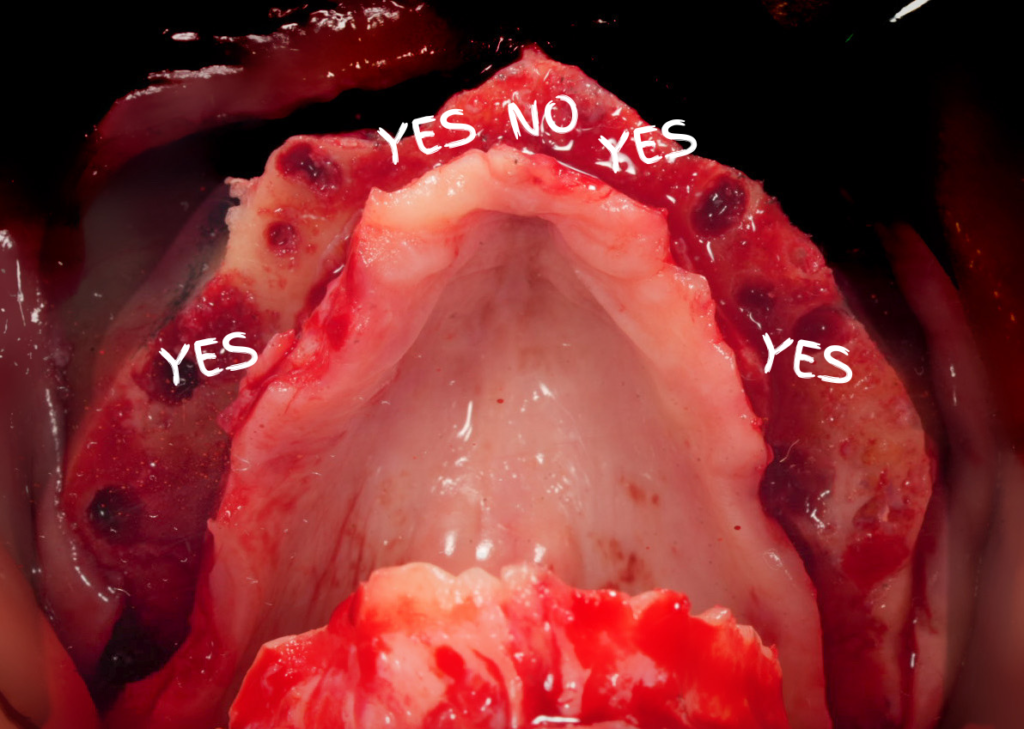
7. An anterior implant failure can negatively affect the adjacent implant.
Over the years I have been referred a number of cases where the patient has presented with a 5 implant, midline configuration and an anterior implant failure.
Unfortunately, the anterior three implants are often placed so close together that the failure of any one of the anterior implants negatively affects the adjacent implant/implants.
For example, let’s say that implant #26 has failed and has notable bone loss and/or acute infection now affecting the adjacent midline implant. While #26 is mobile, the midline implant is compromised but still integrated.
The unfortunate part of this scenario is that if you just had implants #23 and #26 you could have more easily removed the failed #26 and redirected a new implant into a healthy, intact bone site. However, now you have a failed #26, a compromised midline implant with a defect, and little to no real estate to work. This has now become a much more difficult situation to handle.
Furthermore, you cannot just leave the patient on the remaining 4 implants without intervention, as implant #24 now has a significant bone defect and is on its way to failure.
Instead of a single “remove and replace” surgery…we now have to remove #26, perform a ridge augmentation graft at both sites #24/26, bury the midline implant for predictable graft healing, and then return to uncover implant #24 and perform implant placement of #26 in 4-6 months +/- immediate loading depending on implant stability at the graft site.
And all this because we have a midline implant in the way.
It is my opinion that the vast majority of the time, the midline implant provides little to no benefit to the patient or surgeon.
Furthermore, I believe that it can actually negatively impact your surgical outcomes, especially if a future anterior implant replacement is required.
And if that’s not enough…financial math indicates that it is simply a poor business decision.
Here’s to jumping off the Midline Implant Train….
Matthew Krieger DMD
Reference:
Daudt Polido W, Aghaloo T, Emmett TW, Taylor TD, Morton D. Number of implants placed for complete-arch fixed prostheses: A systematic review and meta-analysis. Clin Oral Implants Res. 2018 Oct;29 Suppl 16:154-183. doi: 10.1111/clr.13312. PMID: 30328199.

Love reading your posts! Clear and well thought out (and I find they agree with my philosophy 99%!)
Hope you are doing well!
Thanks Jeff! I’m glad you’re enjoying them! Thanks for the feedback and support!!
Pingback: Why & How I Keep an AOX “Arch Log” - AOX Surgery
Pingback: My AOX Bruxism Protocol - AOX Surgery
Pingback: How I Handle Fractured Roots & Root Tips During AOX Surgery - AOX Surgery
Pingback: Twenty AOX Pearls, Thoughts, & Reflections - AOX Surgery