I exclusively use a tapered implant for All-On-X surgery.
And by exclusively, I mean 100% of the time.
While most implant options today are tapered, there are still parallel walled (and/or very minimally tapered) implants in use and preferred by some doctors. One reason practitioners lean toward a parallel walled implant is that these implants do actually provide a greater surface area and therefore more bone to implant contact.
I feel that the benefits of a tapered implant in the setting of All-On-X surgery, however, far outweigh the increased bone to implant contact a parallel walled implant provides.
In my opinion, a tapered implant is advantageous in every AOX surgical scenario:
- Routine Cases
- Dense Bone
- Difficult Cases with Very Low Bone Density
- Atrophic Cases
Through much trial and error in the scenarios above, I have learned the value the tapered implant provides, especially in regards to consistently achieving a loadable composite torque value.
The key to success with this style of implant is knowing how to utilize the taper effectively.
Let’s take a look below at the significant advantages a generously tapered implant affords an AOX surgeon, that a parallel, or even close to parallel walled implant, simply cannot provide.
Benefits of a Tapered Implant in AOX Surgery
1. Increased surgical flexibility and superior osteotomy site customization – resulting in higher torque values.
This is the single most valuable attribute of tapered implants.
The surgeon is truly in control.
In the hands of an experienced surgeon, a tapered implant provides unmatched flexibility and complete customization of the osteotomy site.
As the surgeon, this allows you to under-prep significantly, slightly, or not at all (and everywhere in between) depending on your tactile sensation of the bone density.
You have this incredible flexibility, because with an aggressive taper, the apical tip of the implant is often a 30-50% reduction in size as compared to the rest of the implant body.
Therefore, even if the osteotomy (or a portion of the osteotomy) is notably smaller than the implant body, the tapered apical portion of the implant can still engage the under-prepared bone and continue down the osteotomy path, increasing torque the further it travels.
With a parallel, or near parallel walled implant, you cannot under-prep the osteotomy in this fashion, unless the surrounding bone is extremely soft.
If you attempt to customize or under-prep your osteotomy with a parallel walled implant, you will run into many instances where the implant will feel like it is torquing well and then all of a sudden it will “spin out” to a torque of zero. This is due to the wide implant apex being unable to pass through the under-prepared portion of your osteotomy.
I can tell you firsthand, this is a terrible feeling when this happens during a difficult case.
With a tapered implant, however, under-preparing your osteotomy site is simply easier and more predictable. This is because you can truly customize your osteotomy site to your tactile feedback of the bone density and then rely on the tapered implant tip to work its magic as it progresses down the osteotomy.
My torque values are typically 45-60 N-cm, and this is almost exclusively due to strategically under-preparing my osteotomy sites and allowing the tapered implant to engage apically and increase the torque value as it progresses through the osteotomy.
2. Increased ability to engage cortical bone sites in atrophic or low bone density cases.
Many implant companies market implants that are less tapered with wider, aggressive threads for low bone density scenarios. However, I feel many AOX practitioners reach for these implants too often in “difficult” and atrophic cases. In my experience this is a mistake…
In atrophic and/or low bone density cases my go to is almost always (99.9%) going to be my “routine” tapered implant (not a “soft bone” implant). And furthermore, I will select my more aggressively tapered implant. Not more aggressive threads, but a more aggressive taper of the implant tip. Why?
AOX surgery requires a minimum composite torque value of 120 N-cm to predictably load. This means AOX surgeons must think a little different when it comes to stability and torque than providers who are placing single implants.
Given this requirement, in atrophic or low bone density cases, I am not typically thinking less tapered, wider, more aggressive implant threads.
I am thinking… cortical bone engagement.
In the more commonly atrophic maxilla, this means the piriform rim, the vomer/nasal crest, the pterygomaxillary pillar, a palatal root socket etc.
In these scenarios, I can slightly under-prep my osteotomy as it travels through soft bone and engages the denser cortical bone in the regions listed above.
The aggressive implant taper I have, will allow my chosen implant to travel through the entire osteotomy while still engaging the dense, but slightly under-prepared cortical bone – without spinning out!
This technique will consistently create torque.
However, trying to use this under-preparation technique to engage these areas of cortical bone with a parallel walled implant – or even an only slightly tapered implant with more aggressive threads – will simply not work. The parallel walled implant will spin out. And you may lose your only chance at loading that case.
In mandibular cases that present with severely low bone density, I will go to a wider implant size (5, 6, or even 7mm) to engage the buccal and lingual cortices to improve torque. However, I still use the same tapered implant and under-prep my osteotomy in a similar fashion. It is simply a wider, tapered implant.

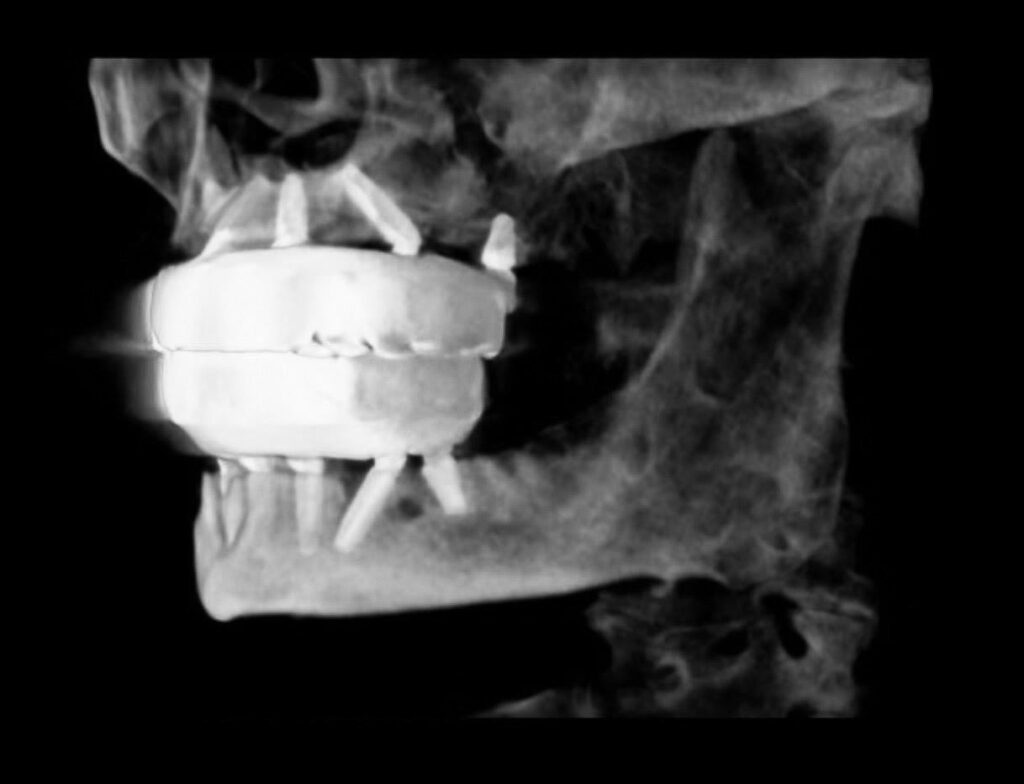
3. Reduced risk of implant apices touching during the use of “M” or “Inverted V” configurations.
In atrophic cases, it is not uncommon to have the apices of your implants very close together.
In these cases it is often advantageous to use configurations such as the “M” or “Inverted V”.
While highly advantageous configurations in my opinion, placement of implants in this fashion can result in implant apices that touch. While this is not the end of the world, in an ideal scenario the implants would not be in such close proximity.
The primary reason is that in the event one implant has an infection and/or needs to be removed, the adjacent implant in contact can be negatively affected.
Contact of implants during insertion can also lead to an implant spinning out during placement.
While a subtle difference, sometimes the simple taper of an implant apex can prevent this contact.
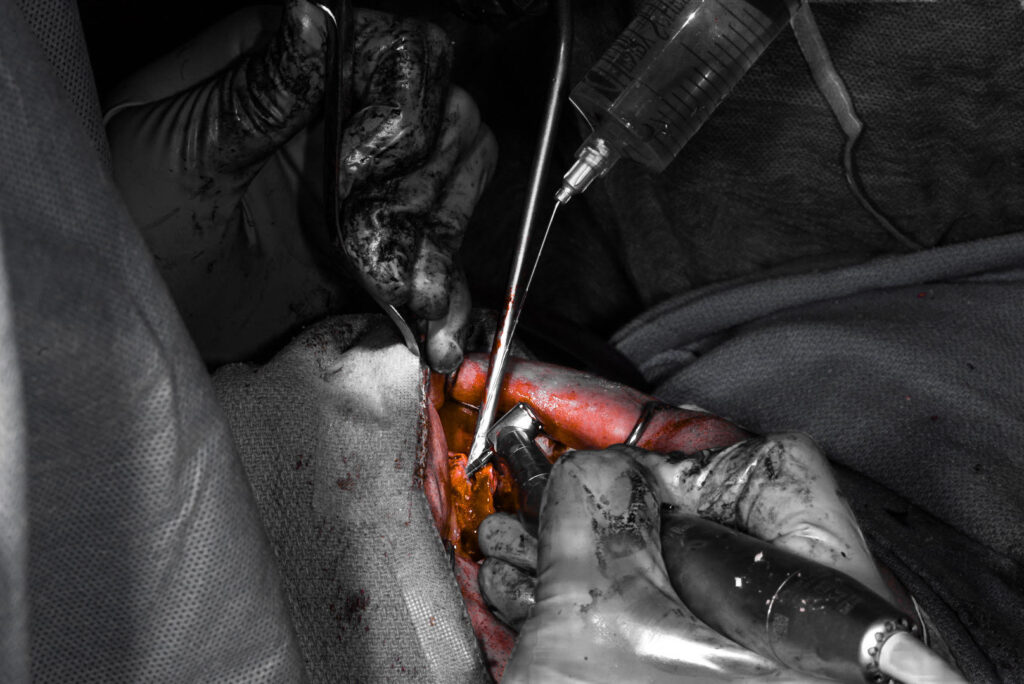
4. Consistent, successful implant placement and high torque values in palatal root socket sites.
A slightly underprepared palatal root site is a magical thing for a tapered implant.
This site generates great torque, improves A-P spread, and is quite simply one of the best tools you can have in your toolbox.
Trying to use this site with a parallel walled implant, however, typically creates one of two scenarios:
- Due to the conical shape of the socket and dense palatal bone, the parallel walled implant spins out.
- You have to drill to full depth and implant size to place the parallel walled implant, leading to very low torque values at this site.
Well there you have it.
There are simply too many advantages a tapered implant gives you that a parallel, or even close to parallel walled implant, just cannot provide.
This is why I feel that the tapered implant is simply unparalleled in AOX Surgery…
Matthew Krieger DMD
P.S.
This article is clearly written exclusively for AOX surgery. These advantages do not necessarily translate directly to single implant placement, especially in the setting of a delayed load.
P.P.S
Some “tapered” implants really aren’t that tapered if you actually look at the thread design. A tapered body with very wide threads, which I commonly see, defeats the purpose for the techniques discussed in this article. I have had the most success with an actual tapered tip or apical 1/4 of the implant where both the tip and threads are truly tapered.


Really love this blog!
Thanks for the feedback and support!
Amazing tips love every single post on this blog
Thank you for sharing your experience with us and thank you for your implant ninja courses I love it!
Matteo – thanks for the feedback and support!
Just started following on Instagram and appreciate the blog!
Thanks Mark! I appreciate that!