I always attempt to perform both the maxillary and the mandibular bone reductions, prior to beginning my implant placement.
Ok, full disclosure: There are a few select instances where I will not do this – and I will discuss these in an upcoming article.
That being said, the vast majority of the time I strategically perform both bone reductions before I move onto implant placement.
This is as opposed to performing one jaw at a time, all the way to surgical completion, and then beginning the next jaw.
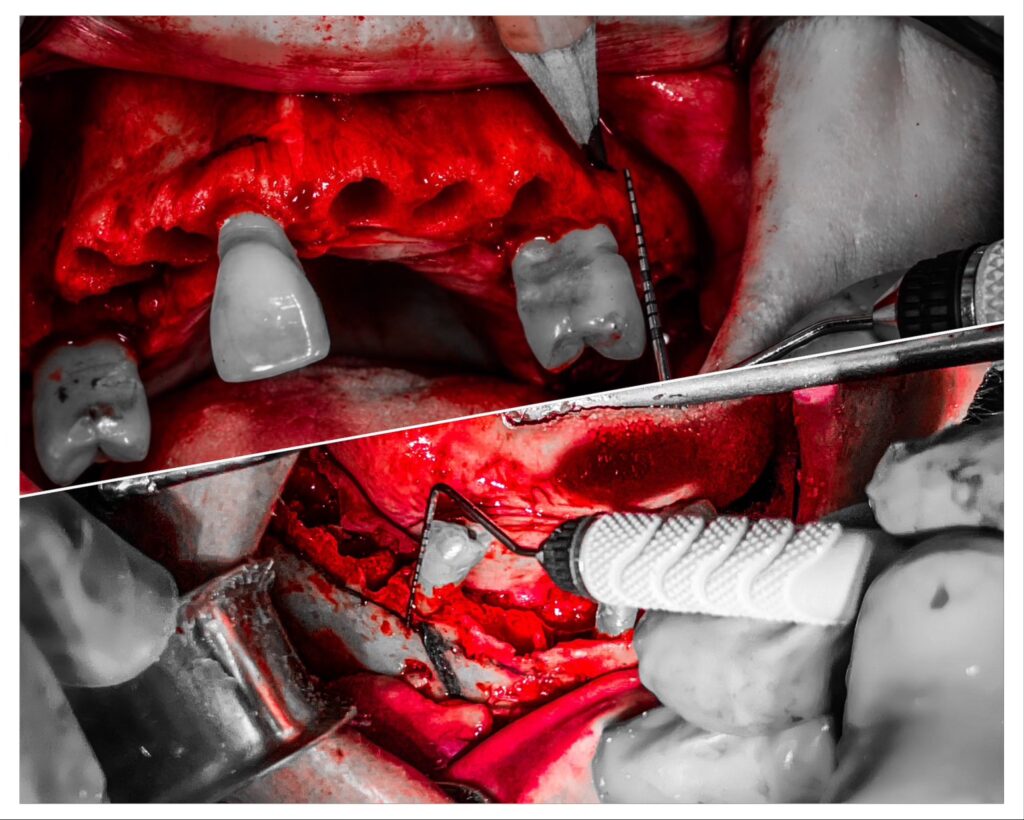
To visualize this process, here’s an outline of the initial steps of my double arch surgery:
- Remove all maxillary teeth.
- Perform maxillary incision.
- Reflect maxillary flap.
- Complete maxillary bone reduction.
- Remove all mandibular teeth.
- Perform mandibular incision.
- Reflect mandibular flap.
- Complete mandibular bone reduction.
- Now I move onto performing my implant osteotomies…
There are 5 key benefits to performing surgery this way that I will discuss below.
Benefits to Performing Reduction on BOTH Jaws Prior to Implant Placement
1. Performing reduction on both jaws prior to implant placement sets us up for a more efficient surgery.
The improved efficiency actually has nothing at all to do with the reduction itself. The benefit, however, comes on the back-end when we are ready for implant placement. With both flaps reflected and both jaws reduced, we are able to drill all osteotomies (upper and lower), place all implants (upper and lower), and position all abutments (upper and lower) at the same time.
Being able to perform these surgical steps on both jaws at once saves a huge amount of time because it allows us to pick up and use the starter drill once, the 3.5 mm drill once, the implant insertion driver once, etc
Attempting to use an instrument once, as opposed to picking it up and putting it down multiple times during the same surgery, is at the core of an efficient surgeon and surgical team.
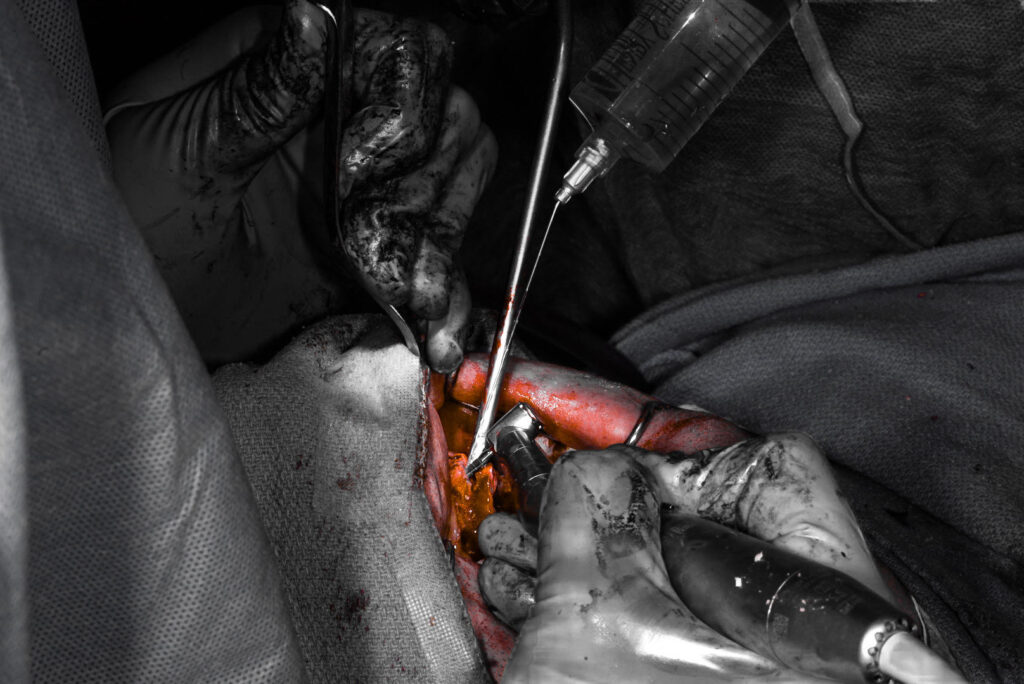
2. Performing reduction on both jaws prior to implant placement creates increased surgical space for our handpiece and implants.
We’ve all been there – trying to cram a larger bite block in, having our assistant hold the jaw open wider, or asking an awake patient to stretch open just a little more.
It can be difficult to fit the implant handpiece, especially with a loaded implant, into the posterior aspect of the mouth without hitting the opposing dentition. This usually leads to having to adjust your desired angulation to a less desirable implant trajectory.
The solution in a double jaw case – perform both bone reductions prior to implant placement. With all of the teeth out and both jaws reduced you will have ample space for your handpiece, drills, and implants – without any interference. It is literally a night and day difference.
3. Performing reduction on both jaws prior to implant placement allows for an accurate intra-operative VDO check.
Confirming accurate intra-operative VDO is an important step to performing high-level AOX surgery.
When cutting one jaw at a time – it is often difficult to accurately assess intra-operative VDO. This is because we are trying to check a reduced maxillary jaw against a dentate mandibular jaw (or vice versa) – with a patient dentition that will no longer be present on the final prosthetic.
An accurate VDO can really only be assessed in a double jaw case with both the new upper and lower prosthetic guides in place.
The only way to have access to both jaws and both guides at the same time, is to perform both bone reductions at the same time.
4. Performing reduction on both jaws prior to implant placement allows the surgeon to view and assess both bone reductions together to compare symmetry and confirm a flat plane.
Following reduction of both the maxilla and mandible, we are now able to stand at the head of the patient and look directly down into the oral corridor. From this vantage point we can easily and effectively compare both the upper and lower jaw reductions.
In this scenario we are able to assess for a symmetrical flat plane on both jaws. If one jaw is uneven, lumpy, or canted – it is far easier to appreciate when compared to the opposing jaw.
This technique helps create and ensure a uniform upper and lower reduction.
5. Performing reduction on both jaws prior to implant placement allows the surgeon to better view the post-reduction maxillomandibular relationship.
Depending on the amount of bone reduction required, the maxillomandibular jaw relationship can and does change slightly. A class II relationship can become more noticeably class II. On the other hand, it may improve to some degree and appear more class I. A class III jaw relationship, in the same manner, can become accentuated after reduction and/or improve, moving toward a class I relationship.
AOX implant position should always account for the jaw relationship at hand. And, assessing the final skeletal relationship is never easier than it is following the reduction of both jaws. Understanding this relationship, and accounting for it with our implant position and angulation, will help to optimize our access holes and provide the patient a more ideal prosthetic.
Here’s to a ‘reduction’ in your surgical stress and a surgical workflow as smooth and consistent as your bone shelf.
Matthew Krieger DMD
P.S. I perform this technique with the patient in a general anesthetic state, with anesthesia administered and maintained by a separate anesthesia provider. This allows me a great deal of flexibility in performing surgery this way – and less stress regarding the effectiveness of local anesthesia. I do not think this technique is feasible or advisable if you perform this surgery with local anesthesia or IV conscious sedation as you may run into difficulty maintaining an adequate level of local anesthetic pain control for the duration of the case. In fact, in these scenarios, I myself would perform one jaw surgery all the way to completion prior to starting the opposing jaw.

Great article, definitely opposite to how I learned it. How do you measure VDO with no teeth on both arches? Can you please elaborate on your local anesthetic protocol. Thank you so much
Hi Marina,
Thank you for the feedback. In response to your questions please see below:
1. Due to the complexity of addressing VDO as a topic/question, I will be discussing this in detail in my upcoming online course. I have also discussed VDO in a previous newsletter. Please keep your eyes out in the future as I am looking for a way to provide access to previous newsletters. It is hard to provide you an adequate, detailed response in this reply (without writing an entire article here).
2. *I have local anesthesia in my queue of topics to cover so please stay tuned. Thanks!
Excellent Info
Thanks!
Pingback: When and Why I Will Cut One Arch at a Time - AOX Surgery
Pingback: Why I Don’t Routinely Bone Graft During AOX Surgery - AOX Surgery