I recently received an intra-op phone call from a colleague, a twinge of stress in their voice, asking what to do if they couldn’t get primary tissue closure for their All-On-X case.
While not a common problem, difficulty achieving primary closure can occur. I want to share with you the advice I provided my colleague in regards to how I would manage this situation. Furthermore, I want to discuss why this scenario may occur to begin with, in hopes that you can avoid it all together on your AOX journey.
Difficulty achieving primary closure? How you might have gotten yourself into this situation in the first place…
1. Removal of too much tissue during your incision.
This is the most common and obvious reason this can occur. If you remove too much tissue, you simply have inadequate available tissue to close over your wound.
Your incision and subsequent tissue removal are two of the most underrated, yet most critical aspects for a well planned, smooth closure.
Remember that the goal is to remove the interdental papilla, along with any diseased tissue, while creating a flat margin along your incision edge. This must also be accomplished without removing an excessive amount of keratinized tissue. Why?
- This allows for a smooth tissue margin but also leaves enough tissue behind for an easy and predictable primary closure.
- This also ensures that enough keratinized tissue remains around your abutments for proper short and long term healing of your implants.
2. Mismanagement of tissue during an edentulous case.
Edentulous cases typically do not require any tissue removal at all.
Ok…never say never.
There are a few cases that will require some tissue removal for a pristine closure. But this is not common.
By nature, most edentulous cases are atrophic. Some bone reduction is normally required, but usually this is not extensive.
Since your bone reduction is often minimal, you simply do not routinely need to remove tissue to create a well approximated closure.
If you remove tissue during your incision on an edentulous case, you run the risk of not having enough tissue to close, or having to put a lot of tension on the wound to get primary closure.
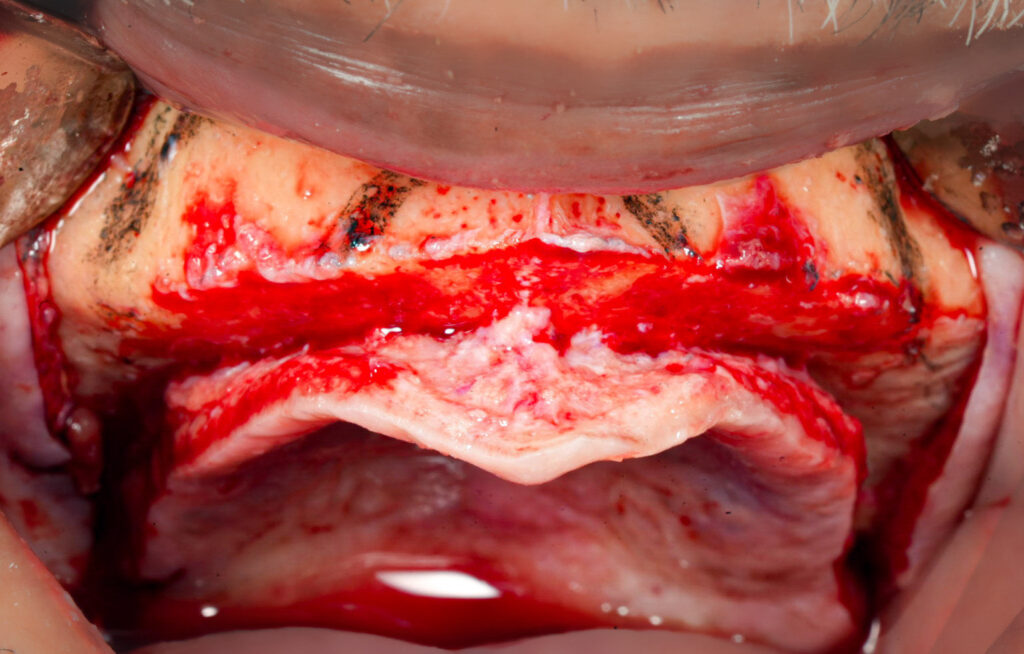
3. Inadequate bone reduction.
If you are consistently unable to primarily close your entire incision line – and you are not removing too much tissue – then you are not reducing enough alveolar bone. Plain and simple.
Even if you are loading your cases, I would bet money that your prosthetic is thin, prone to fracture and inadequate.
It should be exceptionally rare that you have difficulty achieving primary closure if your bone reduction is adequate.
Ok, so we understand how to avoid this situation in the future. But somehow we are in this conundrum today…
So what do we do if we are having trouble getting primary closure??
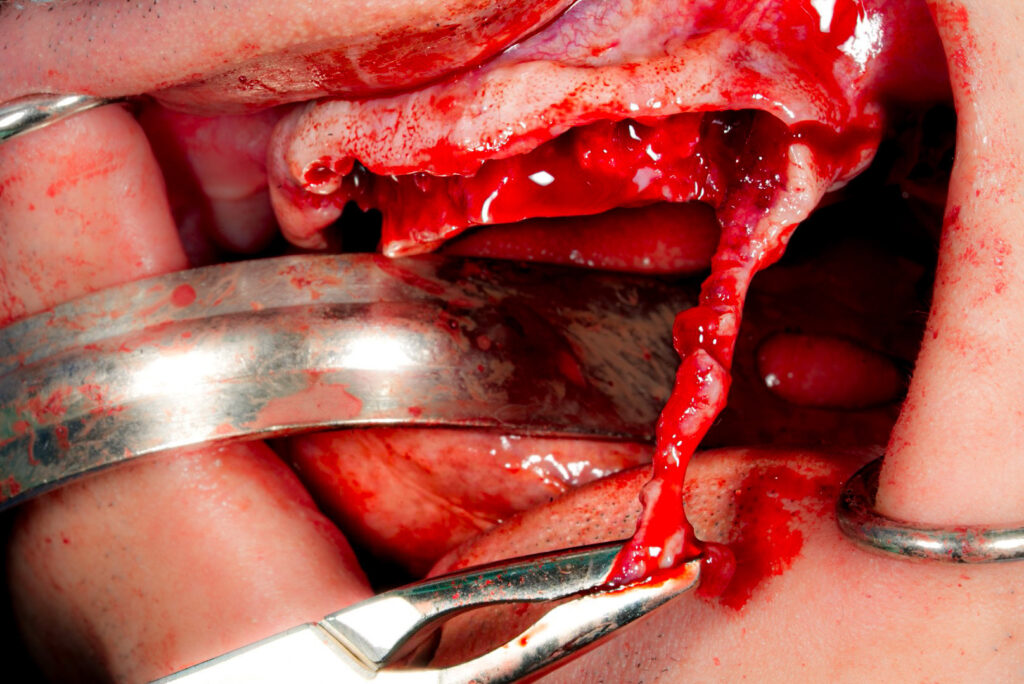
1. Score the buccal periosteum to allow laxity in facial tissues.
This technique will seem obvious to most oral and maxillofacial surgeons, but it is the logical first step and warrants being on this list.
Scoring the periosteum will allow the buccal mucosal tissues to expand slightly when tension is applied. This creates the ability for you to “pull” the tissue over the wound.
If you are not familiar with this technique please ensure proper training and understanding of anatomy as scoring too deeply can damage anatomical structures in the area.
This may be all you need to do to achieve primary closure depending on the extent of the coverage required.
However, keep in mind that you can put too much tension on the wound by pulling the tissue to achieve primary closure. Even if you do achieve wound closure, with excess tension you run a higher risk of the wound dehiscing.
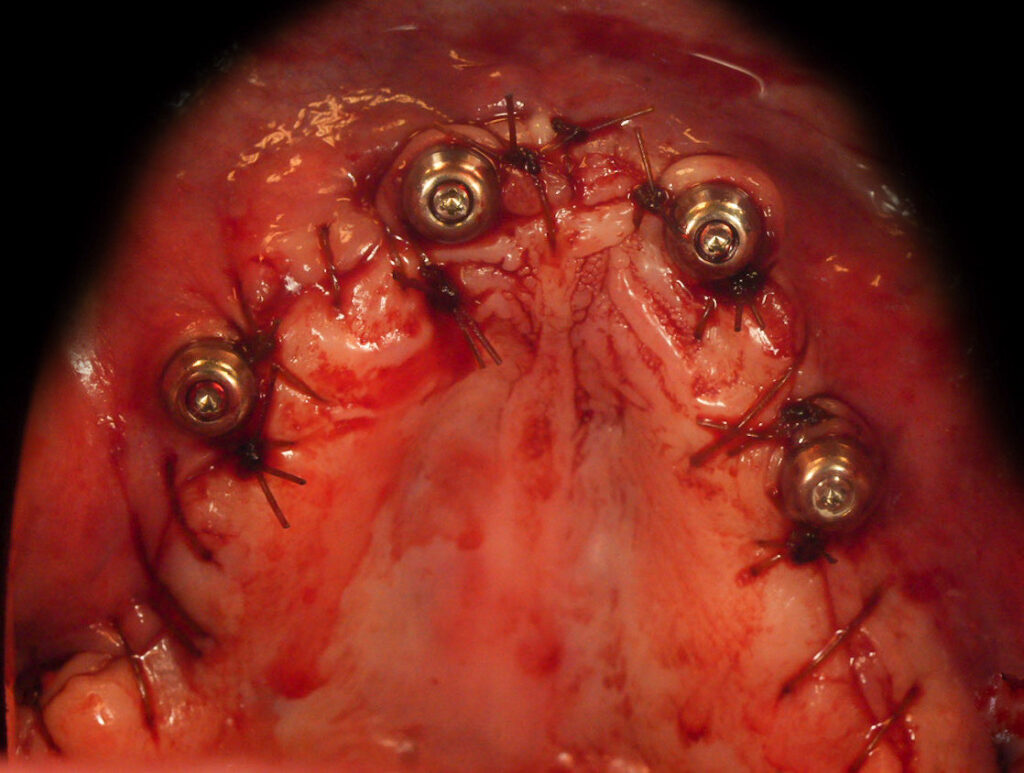
2. Place PRF over/around the implant abutments and exposed alveolar crest.
If I was truly unable to achieve primary closure at a surgical site, my next step would be to get “coverage” of those sites with PRF.
Here’s what I would do:
Flatten the PRF clots into “sheets”.
Next, take a 15 blade and create a small puncture in the middle of the flattened clot.
Then drape the clot around each abutment so that it sits over the abutment and covers the bone around the implant in all directions.
Take any additional clots and place them on top of the alveolar crest in any exposed areas.
While this will not solve your problem, PRF will provide enhanced healing factors to the area, hopefully improving the speed with which you may be able to granulate tissue into any areas not primarily closed.
This technique also provides some post op comfort to the patient as there are less areas of directly exposed bone. Note that I have used this technique successfully and with improved patient comfort when managing a post-op dehiscence.

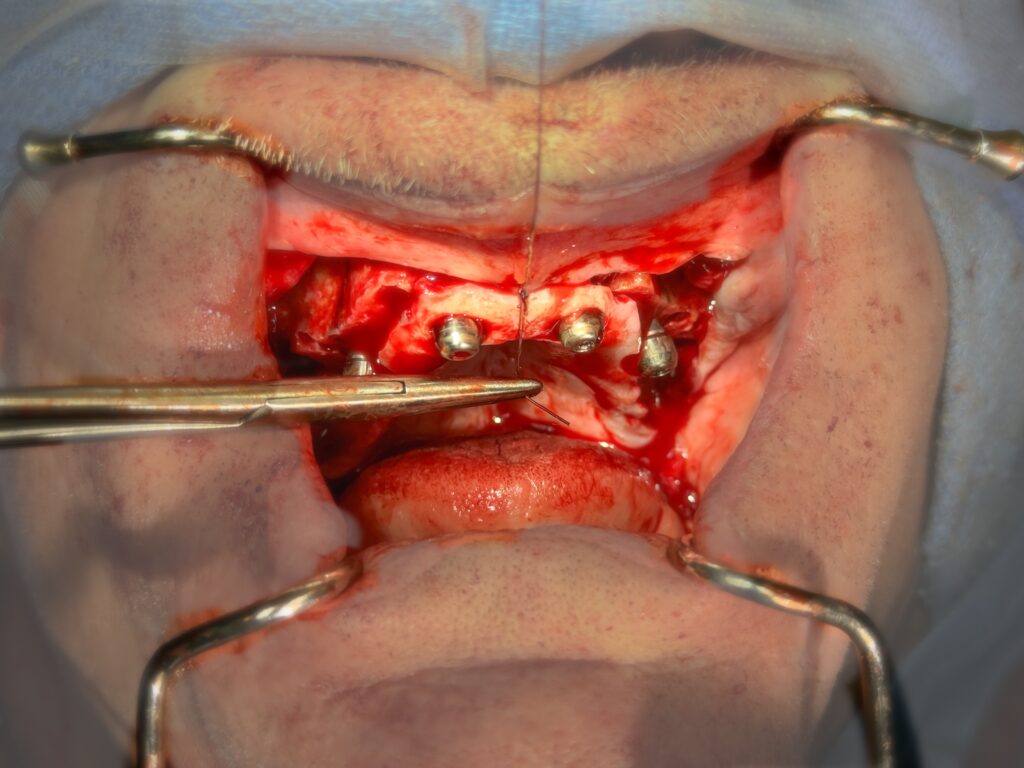
3. Add a long lasting suture like Vicryl to your closure.
Whether you have achieved closure with tension, or have open areas overlaid with PRF, I would add in a longer lasting suture to help hold the wound closed, or nearly closed, longer.
In my practice, I would use Vicryl in addition to chromic gut for this purpose.
4. Ensure antibiotic and chlorhexidine coverage.
This should go without saying, but ensure you have adequate antibiotic coverage during the immediate post-op period to help ensure an optimal state for tissue healing and secondary granulation.
I will note that in this immediate post-op scenario, I will cover with oral antibiotics. However, should an incision that was closed primarily dehisce later in the post-op period – I will not necessarily add additional PO antibiotics unless there is evidence of acute infection.
I would also encourage post-op chlorhexidine rinses to help with secondary tissue granulation.
5. Avoid the use of a waterpik until primary closure has been achieved.
As a surgeon this may not be on the top of your list – but this is very important to help ensure the patient has a fighting chance at achieving primary closure.
Use of the waterpik with an open wound will continually push the tissues apart and dissolve the sutures more quickly than desired.
I would reinforce to the patient the importance of not using a waterpik until the wound heals primarily. You will need to confirm closure visually and inform the patient personally when they can begin waterpik use.
During the healing period I would have the patient continue chlorhexidine and salt water rinses, as well as gentle irrigation of both under the prosthetic with a monoject syringe.
6. Close follow up.
If you are truly unable to get primary closure, the patient should be followed until primary closure is confirmed. The follow-up schedule depends on the extent of secondary healing required and the timeline in which the patient is able to achieve it.
It may look something like this:
- Surgery
- 1 week follow up
- 2 week follow up
- 4 week follow up
- Final confirmation of all sites closed at 6 week follow up
I hope you do not find yourself in this situation. But hey…things happen. No surgery or surgeon is perfect.
If you do find yourself in this pickle, feeling like you’re under quite a bit of “tension”… I hope this article helps you out a bit.
Matthew Krieger DMD

Pingback: How Should I Manage an AOX Post-Op Wound Dehiscence? - AOX Surgery