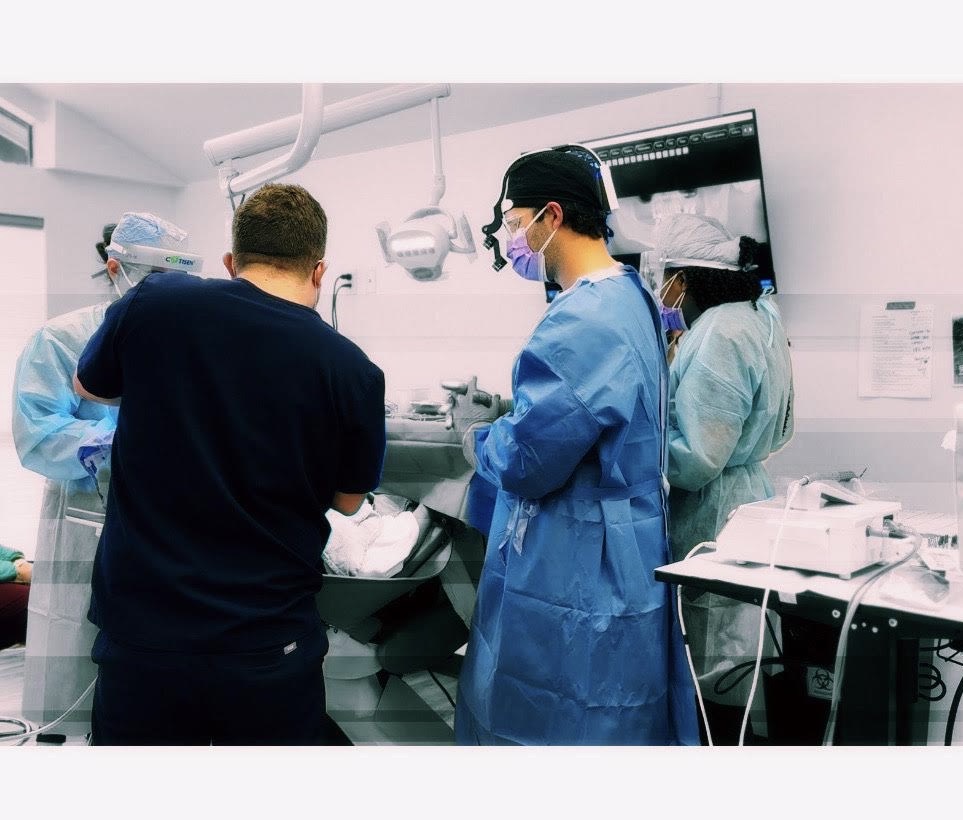
AOX surgery is a team sport. There is simply no way around it.
For those of us in a referral relationship, one of the most important aspects of the full-arch team culture is the ability of the surgeon to work with – and not against – their referring restorative doctor.
It is always easy as surgeons to assume that we will perform the surgery “where the bone is” and the restorative doctor will then be amazed and thankful at our incredible work and the referrals will then flow endlessly…
Well, I’m sorry to burst that bubble, but that’s just not the case.
Fortunately though, there are 4 key areas that we as surgeons can focus on optimizing in order to give our restorative colleagues a more ideal prosthetic outcome – and these will likely lead to more referrals. These are ways in which we can “work with our restorative referral & not against them”.
How to Work With Our Referrals & Not Against Them
1. Pre-operative communication and treatment planning.
I would assume that this goes without saying. But I would be wrong.
I have experienced, seen, and been informed of instances of an incredible lack of communication amongst providers in the full-arch world. I would like to add that this is often worse in the “traditional private practice world” where providers are in different offices and busy with their own day to to day.
In order to improve pre-op communication, it is my preference that an AOX Surgical RX be provided to the surgeon by the restorative provider. This will guide the surgeon in understanding the restorative provider’s prosthetic requirements and vision for the prosthetic.
This is so important because it opens the dialogue between the surgeon and restorative provider.
Now that the surgeon can visualize what is required restoratively, they can start to discuss with their prosthetic colleague what is realistic surgically. This includes what may not be doable, and where they may need to “meet in the middle”. In this way, there should rarely be surgical surprises.
In order for this to be effective, it is a two-way street. As surgeons, we cannot provide our restorative colleague an “ideal” outcome if they have not informed us what “ideal” is for that case.
But – if we do have one of those wonderful referrals willing to provide us this information (AOX Surgical RX) as part of their work-up, it is OUR responsibility as surgeons to review it and discuss the surgical impact with our colleague.
We need to be open about what kind of a final result we can deliver based on their prosthetic requirements.
2. Elimination or minimization of the cantilever.
While we typically envision the cantilever as a surgical issue, it is also a prosthetic issue.
Not only can an increased cantilever lead to implant failure, but it can also lead to prosthetic fracture. This is due to masticatory forces at unsupported weak points in the prosthetic created by the cantilever.
So, ok… we all get that a large cantilever is bad but what does this have to do with working with and not against our restorative referral?
Well, after we do our surgery and send the patient back to our restorative colleague, guess who gets to see that patient every 3-4 months for a prosthetic repair when it fractures…?
Our implants may very well integrate. But our AOX referrals may also drop off when our restorative colleagues get burned out and tired of this “full-arch stuff” while they are spending consistent parts of their production days repairing fractured prosthetics.
3. Minimize lingual and palatal prosthetic “bulk”.
This is not something that most surgeons think about. And I get it. The focus is on implant stability, torque etc.
But knowing where our implant access holes come out on the prosthetic will set us apart amongst our referrals.
This is one of the ultimate ways to work with and not against our referral. This is a true sign of an experienced and/or talented AOX surgeon.
Why?
Again… we may place 4 or 6 implants that have great torque and all integrate. But if we place them too palatal or too lingual – I promise that for the next decade, all our referral is going to hear at every single follow-up appointment is,
“Why is there this big thing on the roof of my mouth? Why is it so bulky? I don’t like this at all. Can you change it? This is not what the example looked like…”
Working “with” our restorative colleagues requires providing them as ideal access holes as possible.
4. Assessing and compensating for a class II or class III skeletal discrepancy.
While we will discuss management of patients with a skeletal discrepancy in a future article, realizing that they present with a discrepancy and how that impacts both a surgical and prosthetic plan is key to an optimal outcome.
If we do not account for the skeletal discrepancy surgically, we will create significant excess prosthetic bulk on one or both jaws.
This occurs because the restorative doctor will attempt to move the prosthetic into an “ideal” position to correct the jaw discrepancy. This usually requires moving the prosthetic beyond the bony envelope and therefore creates a large disparity from where our implants exit the alveolar crest and where the actual dentate portion of the prosthetic lies. This will create significant prosthetic bulk.
And, as we have discussed above, this “bulk” is not something that patients (or restorative doctors) appreciate.
I want to acknowledge that all of the points above have both surgical and prosthetic attributes and therefore also have responsibility required from both parties involved in order to optimize the surgical and prosthetic outcomes.
However, being that I am a surgeon and focus solely on the surgical aspect of AOX, this article is written from that viewpoint.
This article highlights the areas in which we as surgical providers can improve our working relationship with our referrals for better communication, better surgical and prosthetic outcomes, and ultimately more AOX referrals.
Whether we like it or not – here’s to working as a team.
Matthew Krieger DMD