It happens.
Sometimes implants fail.
Ironically, whether you work in a DSO style full-arch practice or a traditional private practice, it is often the restorative provider who first notices a potential failed implant upon “prosthetic follow-up” – not the surgeon.
As such, I have created a Failed Implant Protocol to help guide my referrals on how to confidently manage the first steps of identifying and initiating the treatment process for a failed full-arch implant.
This flowchart is shown below and highlights how I prefer my referrals to handle a potential implant failure when noted at a prosthetic appointment. The goal is timely, practical, and optimal management of the surgical patient.
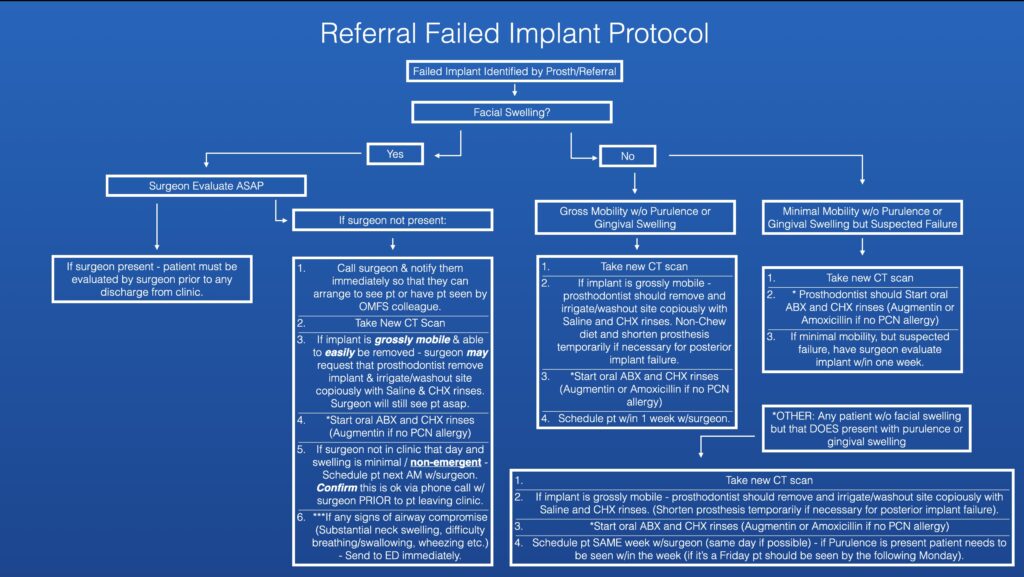
Despite the flowchart, I want to point out that responsibility for surgical management of the patient always falls on the surgeon. However, as discussed, this procedure is truly a team sport and it is actually more common for a restorative provider to note a failed implant at a routine follow up than it is a surgeon to note a failed implant at a surgical follow-up.
A patient may even present with discomfort at a restorative follow-up and have a failed implant inadvertently removed with the prosthetic during the exam. Many restorative providers are uncertain and uncomfortable with how to handle these situations.
In my experience, this guide has helped provide confidence to the restorative doctor and therefore instill confidence in the patient that the less than ideal situation at hand is being managed with expertise.
It has also helped my referring providers better understand how I view non-emergent, urgent, and emergent situations.
This outline is not intended to make restorative providers manage failed implants on their own, but rather to help them initiate a plan for care, notify the surgeon within an appropriate amount of time, and schedule the patient strategically.
May your failures be few, but may you always be prepared.
Matthew Krieger DMD
P.S.
Depending on your experience and your surgical preferences, it is unlikely that this exact outline will suit your needs. However, you can set up your own flow chart that helps guide your referrals with your own preferences for surgical situation management. It is my experience that this is much appreciated.
As always these are simply my opinions/preferences on how I manage the above situations (in the setting of a dual Prosth/OMFS AOX practice), use your own judgement as a surgical provider as to what you feel is best for you, your practice, and most importantly your patients.
P.P.S.
I would like to add that the prosthodontists I work with are well trained in how to manage a failed implant and do not respond with panic as shown in the “title photo” above. However, their calm, cool demeanor would not have made the point as well for this article…
I would imagine, however, that at one point or another this phone call has likely happened to at least a few of those surgeons in a more traditional referral relationship.