All-On-X surgery is about as big a procedure as is consistently done in the outpatient oral surgery setting. Given the magnitude and transformative nature of the procedure, there is a lot at stake for both the patient and the surgeon.
This incredibly impactful power of AOX surgery is also why this procedure is arguably the most rewarding in our field.
That being said, not every patient is a great candidate for this procedure. There are a number of factors to assess that include medical history, jaw relationship, and multiple anatomical considerations – just to name a few.
One area, however, that is often overlooked is the psychological aspect of full-arch surgery. Moving from natural teeth to a fixed prosthetic can be quite an adjustment for some patients.
Patients don’t often realize that a full-arch prosthetic will lack the sensory feedback they get from a natural dentition, will feel unusual to their tongue (at least at first), will temporarily affect speech, and will sound “louder” than their previous dentition.
Most patients do not mind. This is because most patients have no teeth, and/or very few teeth left and the fixed prosthetic, despite the “downsides” listed above, is a welcomed change.
However, as full-arch surgery becomes more popular (and more affordable when offered at significant discounts by some practitioners), many patients with “restorable” dentitions are moving forward with full-arch surgery.
In a full-arch setting, these cases are arguably more “elective”. What I mean by this is that these patients could receive traditional restorative dentistry and/or traditional implant restorations. However, as is often the case, pursuing these treatments may be as much as 2-3 times the cost of a full-arch surgery and take 12-18 months.
Many patients elect to forego this traditional path in exchange for a full-arch fixed prosthetic.
I want to be clear that I do not think full-arch surgery should be a truly elective procedure.
However, I have operated on my share of “semi-elective” patients who, for any number of reasons, cannot or do not want to pursue traditional dentistry. This is most commonly due to either finances, a significantly prolonged treatment timeline, and/or an extreme phobia of the dentist.
That being said, I would like to insert one pearl of wisdom here:
Semi-elective patients are by far the most difficult patients to please. So tread cautiously when operating in this scenario.
Let’s take a look below as to why I feel we should all pay attention to that yellow AOX caution flag waiving in the wind…
Why Semi-Elective AOX Patients are the Most Difficult to Please
1. Chewing efficiency doesn’t really change.
One of the most significant benefits of full-arch surgery is restoring masticatory function. Most All-On-X patients have no teeth, or very few teeth, and have struggled to eat the foods they enjoy. Many have even lost weight or developed associated medical comorbidities due to an inadequate diet.
Semi-elective patients, however, do not necessarily lack masticatory function. They are often missing 1- 4 teeth, but may also have some significant cosmetic defects, malocclusion, and dental decay necessitating extensive traditional dental work. While it may very well be beneficial for these patients to pursue All-On-X surgery, these patients really don’t see a notable change in masticatory function and chewing efficiency.
On one hand, this is ok. In reality, these patients are seeking other outcomes such as cosmetic enhancement, time savings from a prolonged traditional treatment timeline, and an often significant financial savings as compared to traditional dentistry.
However, because function is not one of the driving factors for the surgical procedure, these patients are inherently more critical of the esthetic outcome as well as the “feel” of the prosthetic. They want the look and feel of the prosthetic to be close to what they are used to with a natural dentition.
This is in stark contrast to a patient who had a removable lower denture that never stayed in place, and now has a fixed prosthetic. They aren’t nearly as focused on the cosmetic aspect or even the “feel” of the prosthetic – they simply couldn’t be happier to have fixed teeth.
2. Many Semi-Elective Patients Want a 2nd Molar Prosthetic.
By nature, semi-elective patients are more dentate. While they are missing some teeth, many will often have second molars or at least some of their second molars.
I have noticed that time and time again, despite any pre-operative discussion, these patients truly miss the feel of having their second molars. Whether or not the second molars are actually providing any enhanced chewing efficiency is irrelevant. These patients are used to the feeling of these teeth and they want them on their prosthetic.
Why is this an issue?
Having second molars tends to make full-arch surgery much more difficult.
Adding an extra tooth to the prosthetic inherently increases the prosthetic cantilever. This often means your surgical plan has to change to account for a second molar while achieving a surgical and prosthetic design that is likely to have long term success.
Keep this in mind when treatment planning semi-elective patients. A second molar not only increases surgical difficulty, but also surgical overhead. This prosthetic design often requires additional implant placement and additional surgical and anesthetic time.
3. Semi-Elective Patients are Often Bruxers.
Ok, ok. This is not a direct correlation.
But, what I am pointing out is that many, many bruxers come in as 40-50 year old patients with the vast majority of their teeth. However, virtually all of their teeth are worn down. While they may not have extensive decay, they have been told by their dentist that they will require a full mouth dental reconstruction with crowns and root canals on every tooth and multiple months of treatment.
While surgery is not this patient’s only option, I agree that most of the time (with the right treatment plan) these patients can benefit greatly from full-arch surgery.
However, they are often a difficult surgery and can be a more complex patient to please.
Why?
These patients normally have most of their teeth, and therefore as mentioned above, often want a 2nd molar prosthetic.
These patients are also usually extensive bruxers, which means this is a more difficult surgery to complete with long term success and requires a higher level of surgical planning.
In addition, there is theoretically a higher chance of implant failure due to increased forces during the integration period. This may lead to a higher failure rate, and therefore redo surgeries, which can be frustrating and hard for these patients to tolerate when they might not have actually had any true dental pain prior to surgery. They are more likely to second guess their decision to pursue surgery in the first place.
Finally, this group of patients may require, or at least benefit from botox therapy. While this does not necessarily create a harder to please scenario, it is simply an extra step for patients to take that may detour from a more “seamless” full-arch experience.
Despite the points above, I would like to say that I do actually treat a high volume of bruxers and have great success. I think these patients can benefit significantly from AOX surgery. But, I feel it is important to consider the points above to ensure an optimal treatment plan, outcome, and patient experience.
4. Semi-Elective Patients Cannot Stand the Feeling of a Bulky Prosthetic.
When patients have most of their teeth, they are used to the feeling of their tongue coming into contact with their natural palate and against the lingual surfaces of their natural dentition during rest, masticatory movements, and speech.
Following full-arch surgery in significantly dentate patients, it can be a more difficult adjustment to transition to a prosthetic. While virtually all patients do adapt with time, this is a more challenging transition if the prosthetic is bulky, with a large palatal or lingual flange. This can be something that is brought up in frustration by the patient at every prosthetic follow-up appointment.
A higher emphasis needs to be placed on optimal implant and screw access position for these patients in order to minimize any prosthetic bulk.
Again, while patients do tend to adjust, it is simply a more difficult and prolonged adjustment for dentate patients. Extra care should go into treatment planning in order to minimize any excess prosthetic material as a means to improve the dentate patient experience and overall satisfaction.
Note that this is a very different scenario from a denture patient or an RPD patient who has the exact opposite experience. They couldn’t be happier and more grateful that the new prosthetic is so thin compared to the removable prosthetic they are used to!
5. Semi-Elective Patients Need to be Immediately Loaded.
The last, and most stressful reason that semi-elective patients are more difficult to please, is that they need to be immediately loaded.
Patients who have most of their teeth, do not want to wear a denture for 4-6 months while implants are buried. I don’t blame them. I would not want to either.
These cases, therefore, actually tend to create a lot more pressure on the surgeon to generate an optimal surgical outcome.
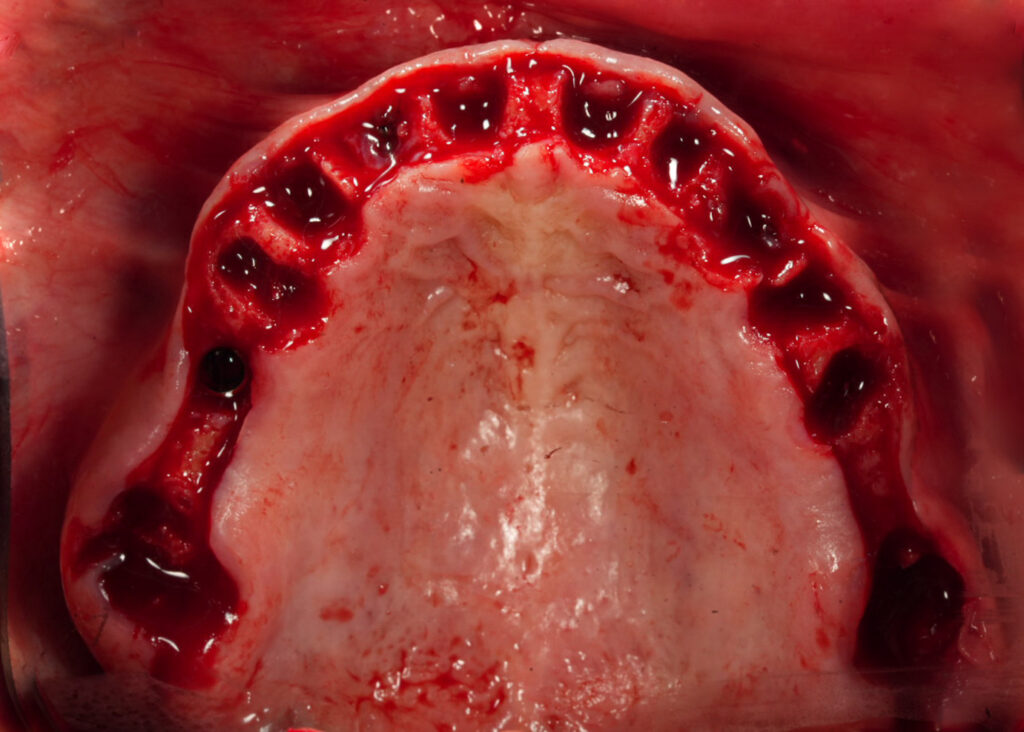
Furthermore, a patient with the majority of their dentition can also give a false sense of an “easy” surgery as they often have a greater amount of bone availabilty.
However, a near complete dentition (especially with worn crown structure and/or root canal therapy) can lead to difficult extractions, increased bone removal, buccal plate fractures, and large socket cavities that can unexpectedly make immediately loading difficult. For this reason, these cases should always be treated with respect.
Semi-elective patients are a subset of patients that have now entered into the full-arch world and are here to stay.
While I do not feel AOX surgery should be a truly elective procedure – semi-elective patients, in the right scenario, can and do benefit from this surgery.
I do not treat all semi-elective patients, but I do treat those that I feel (after assessing all patient factors) will truly benefit from the procedure. However, I do so with a caution and respect, knowing that at no fault of their own – these patients are inherently more difficult to please.
AOX surgical success is found when we know both what our patient wants to achieve through surgery and where they are starting from clinically and psychologically. This will help us know as surgeons if we realistically can or cannot help our patients achieve their smile goals and actually enhance their life though full-arch oral rehabilitation.
My goal in writing this article is not to detour you from treating semi-elective patients. It is quite the contrary. My hope is to help provide you the confidence to know which semi-elective patients you can truly help, and given a different subset of needs, how you can predictably provide these patients a successful surgical outcome with which they will be pleased.
It is wise to remember that,
Full-arch success lies in the perception of the patient, not in the perception of the surgeon.
Matthew Krieger DMD

Pingback: When I Say No… - AOX Surgery