I am fortunate to have the luxury of practicing alongside a prosthodontist. Therefore, in my practice I do not do the prosthetic work-up for our All-On-X cases. And quite frankly, that’s how I prefer it.
I am able to focus solely on what I love, the surgical aspect.
That being said, prior to surgery there are key prosthetic pieces of information that I need in order to be able to provide an optimal, prosthetically driven surgical outcome.
Listed below are the items that I request from the prosthodontist in the form of an “AOX Surgical Rx”. If I was in a traditional private practice, I would request this same exact information from my referring doctor.
For those clinicians that perform both the surgical and restorative aspects, please take note that in my opinion, the following prosthetic information is the most important to have on hand at the time of surgery in order to optimize the surgical outcome.
Furthermore, if you are restorative provider that works as part of a traditional referral relationship, this information is incredibly helpful to provide to your surgeon. In doing so, you will also make your life a lot easier as you are now able to manage a prosthetic created by a well planned, prosthetically driven surgery.
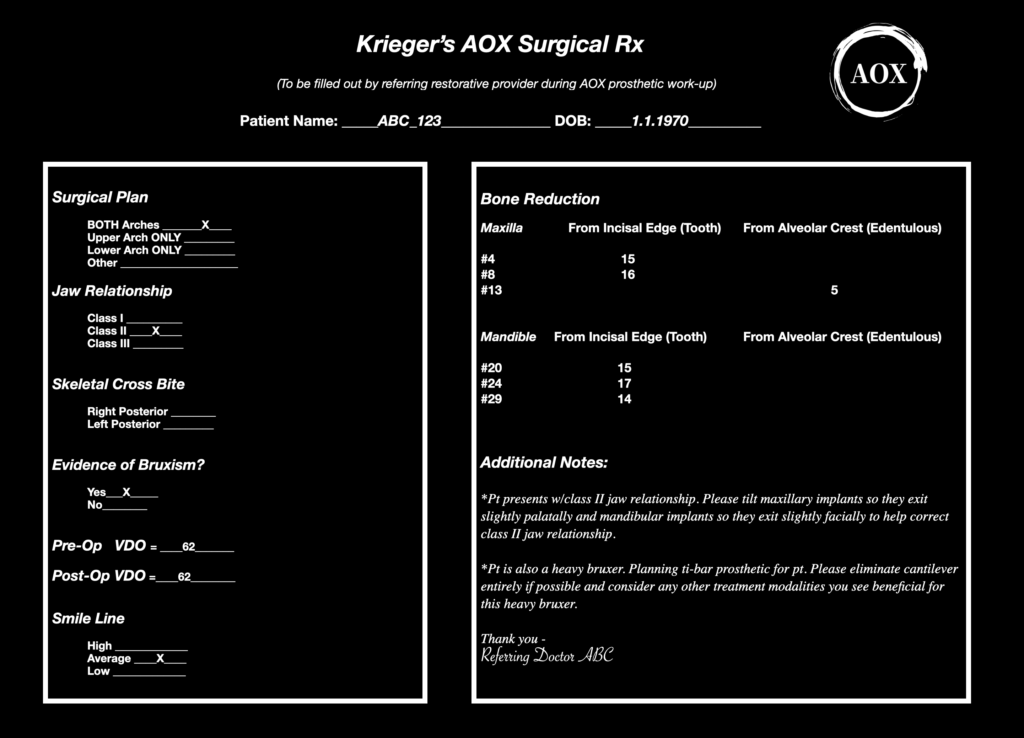
Krieger’s AOX Surgical Rx
Surgical Plan
I want to know exactly what we are planning on doing. I want this very clearly indicated so there is no confusion!
Is it an Upper and a Lower Arch? A Single Arch? Maxilla or Mandible? Is it a Single Arch with isolated extractions on the opposing arch?
There are multiple points throughout the surgical day where this information is confirmed… and confirmed again. And this is yet another point where I can visually confirm that the prosthodontist, myself, and the patient are all on the same page.
It may seem like overkill, but with full arch surgery – you want to ensure there is absolutely no doubt about the surgical plan.
Having an accurate Surgical Rx also ensures the surgical team knows whether one or two arches are planned. This helps them set up instrumentation that is accurate and appropriate for the procedure (correct amount of local anesthetic, sutures etc.).
Jaw Relationship
This is a piece of information that is often overlooked, but is of vital importance in my opinion.
I always want to know if the patient is a Class I, II, or III jaw relationship.
Why?
If the patient presents with a class II or III relationship, I know that to some extent I have to tilt my upper and/or lower anterior implants to compensate for and attempt to correct the skeletal malocclusion.
If I do not compensate surgically, the prosthodontist is still often able to correct the bite prosthetically, aside from extreme cases. But… without accounting for the jaw relationship surgically – the patient will be left with a large chunk of prosthetic material, either on the palate (moving the upper arch forward to correct a class III discrepancy) or on the mandible (moving the lower arch forward to correct a class II discrepancy).
One thing I learned early in my career, was that restorative providers cannot stand when patients come in at every office visit and complain to them about how thick their prosthesis is… and there’s really nothing they can do about it due to the position of my implants.
Accounting for the jaw relationship and subsequent orientation of our implants is a great way to minimize this occurrence!
I would like to add that I am only concerned with a skeletal class II or III discrepancy. A true “dental” class II or III malocclusion will be corrected with removal of the dentition and fabrication of the new prosthetic.
Skeletal Crossbite
The designation of a skeletal crossbite is also an often neglected surgical component. It is easy for us as surgeons to not know (or care) if our patient is in a posterior crossbite.
However, I think that this is a critical piece of prosthetic information for surgeons to be aware of as part of the pre-operative work-up.
And yes, our referrals will likely assume that we can just look in the mouth and see this information. But it is appreciated to have it as part of the work-up provided by the restoring doctor, so that there is a mutual plan on how to handle it.
Now, if this is simply a dentate crossbite, it won’t matter after removal of the dentition and completion of the bone reduction. A true dentate scenario in fact, is not an issue at all. And this may be why it is often not considered as part of the surgical plan.
However, if the crossbite is skeletal in nature, that will very likely still exist after your bone reduction.
This is important for us as surgeons to know, as we can help correct that crossbite surgically with our implant placement.
If my prosthodontist indicates that the patient is in a left mandibular posterior crossbite, I know that on the left mandible I am going to shift my posterior implant/implants toward the lingual aspect of the ridge – not centered in the ridge. This will help bring the mandibular prosthetic arch back to a more normal occlusal position.
Now, in reality, the prosthodontist is likely able to correct a skeletal crossbite even if I don’t shift those implants. In the setting of AOX surgery, this is likely why many of us as surgeons don’t really pay attention to a crossbite.
However, it’s all about style points.
If we can recognize a skeletal crossbite and shift our implants accordingly, we will allow the prosthodontist to correct the crossbite while still having our screw access holes come out of the occlusal surface of the prosthetic. If we do not shift our implants and the restorative doctor corrects the crossbite, the screw access will likely come out of the buccal aspect of the prosthetic. Restorable yes. But they won’t be singing our praises.
Evidence of Bruxism
This is something that we as surgeons should assess ourselves. However, the value in having our referral assess this as well, is having a unified treatment plan to account for and treat the bruxism.
Knowing if a patient is a heavy bruxer is important from both a prosthetic and surgical standpoint.
These patients may require unique prosthetic considerations, such as a final prosthetic material that will account for more strength and longevity given increased bite/bruxism forces.
Surgically, these patients may require additional implants to eliminate a cantilever and may also be considered for things such as botox therapy to limit the incidence of post-op bruxing.
Bruxers require a true team approach for optimal management and outcomes. This is why I feel it is critical that both providers are on the same page with management of these patients.
This team approach starts with the referring doctor noting bruxism on their prosthetic work-up and alerting the surgeon about both the presence of bruxism and the prosthetic plan to account for it.
VDO
A pre-op and post-op VDO are absolutely critical to performing a successful and optimal All-On-X surgery.
If we are not checking VDO intra-operatively – we might as well just practice with the lights off…
In a referral relationship, this information should absolutely be assessed by and come from the restorative provider. This is restorative dentistry at its core and the restorative provider will often be managing the issues related to an improper VDO post-operatively. The restoring provider should want to provide you an accurate pre and post-op VDO to make their life easier in the post-op period.
As the surgeon, the post-op VDO is used intra-operativly following bone reduction to ensure that the patient’s planned “prosthetic bite” has an accurate VDO. If the VDO is off, bone reduction needs to be assessed and adjusted as needed. While there is some wiggle room in VDO – if we are off to much this can create post-operative issues for both our patient and our restorative colleagues.
For reference, the prosthodontists that I work with come in every single case and assess the VDO after I have performed bone reduction on both jaws (this can also be done by the surgical provider). This gives us an accurate, intra-op VDO assessment. If the VDO is not on-point, we adjust surgically to account for that and then re-evaluate.
Smile Line
It is imperative for the surgeon to know where the smile line is located on each patient. I prefer a simple “Low, Average, or High” designation – including an “exaggerated smile photo”.
While ultimately the Bone Reduction #’s should account for the smile line, a quick glance at either a “Low” or “High” designation gives me very important feedback.
If the patient presents with a Low Smile Line, I know that I am likely to require less bone reduction to hide the prosthetic transition line. Furthermore, there is often a plan to increase VDO in these patients which also provides me a greater amount of prosthetic space – and less required reduction.
Now, the one I really pay attention to is the High Smile Line. This tells me that I will need more bone reduction than average and that I need to pay even more attention than usual to the bone reduction to ensure that the transition line is hidden.
For high smile patients, I also prefer that the exaggerated smile photo of the patient is displayed in the operatory, so that I can get a visual picture of where I need to be with my bone reduction.
Regardless of the bone reduction #’s provided, as the surgeon – knowing the smile line designation is important to have in the back of your mind during both pre-operative treatment planning and while cutting the surgical case.
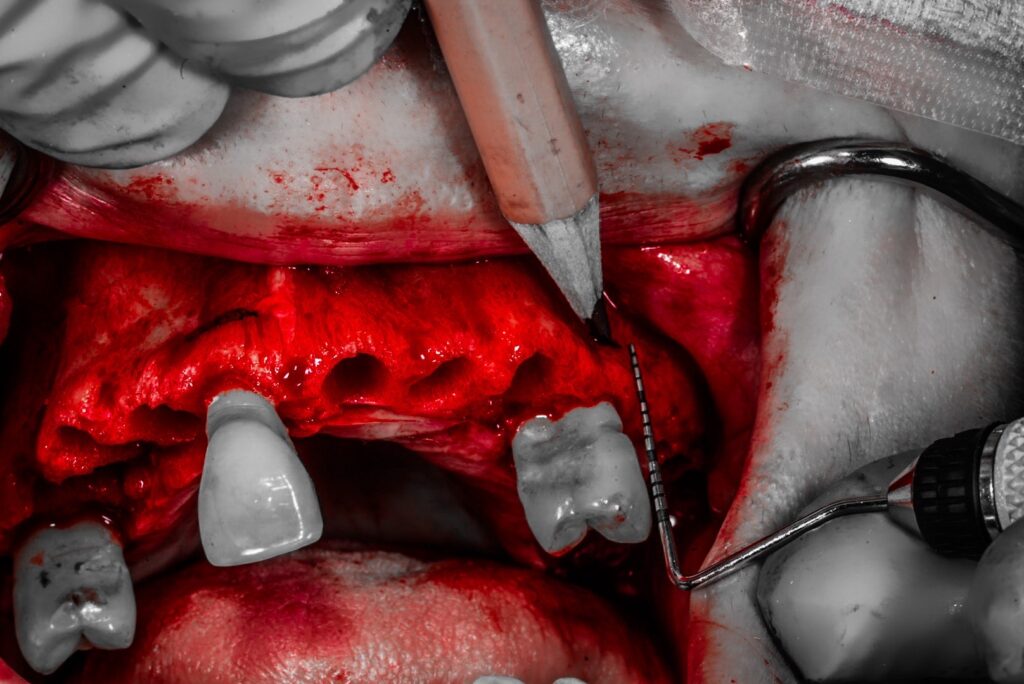
Bone Reduction #’s
I need to know the amount of bone reduction required in order to provide enough restorative space and hide the transition line.
I prefer the prosthodontist indicate the bone reduction required by measuring from the incisal edge of teeth #4/8/13 on the maxilla and from the incisal edge of teeth #20/24/29 on the mandible.
I prefer these sites, as these are typically the locations of “routine” AOX implant placement.
If those teeth are not available, we use an adjacent tooth. If that area is edentulous we will use a measurement from the crest of the alveolar bone.
Typically these numbers will range from 14-20mm depending on the anatomic location and wear of the teeth.
I know that some surgeons do not receive this information from their restorative providers and may arbitrarily do their reduction to account for 15mm of restorative space. While this works most of the time – I do not advise this.
In my opinion, exact bone reduction measurements are important and this information really should come from the doctor who is doing the prosthetic work up and who will be managing the prosthetic after surgery, for years to come. They will have to deal with an improperly hidden transition line or a prosthesis that is too thin and fractures due to inadequate reduction.
In order to prevent the above scenario, I prefer to know exactly what the restoring doctor wants, so that I can deliver a product that both my patient and my referring provider will be happy with.
Additional Notes
This is a section that I provide so that my prosthodontist can notate any additional requests.
Examples might be the following:
Extractions requested on an opposing non-AOX arch.
A reminder that due to a class II or III jaw relationship they would like the implants tilted in a certain direction.
Indicating the patient is a bruxer and requesting additional implants if possible and/or relaying the prosthetic adjustments/plan for this patient.
Below is an example of what an AOX Surgical Rx with the above pertinent referral prosthetic information might look like.
Enjoy! I hope this helps with clarity and consistency in your arches and in communication with your referrals.
Matthew Krieger DMD
P.S.
I would like to add a disclaimer that this is not the form or paperwork that the AOX practice I work for utilizes. Nor is it one that any practice I have worked for in the past has used. While all full arch practices have some way to communicate this type of information (or should) – the form shown is one I have created for myself that highlights only those items I feel most important to me as the surgeon.

I am curious to learn the financial side of AOX if you’d be willing to write an article on it. Average collections per arch vs overhead vs profitability vs income.
Hi RH,
I am fortunate (in my opinion) to have worked the past 5 years for DSO style AOX centers. Therefore, I focus only on what I love – the surgery. This also provides me the volume of 40-60 arches of surgery a month – which is an incredible opportunity for building experience and surgical skill.
I suppose that both a positive and negative, however, is that I have not had ownership in and/or handled any of the marketing or financial aspects of these practices. As such, I do not consider myself an expert in this area and would not want to write about something that I do not feel knowledgeable about.
great points , thank you,
what do you use to measure the VDO intra operative , due you have a denture made before surgery, and if so
with the flap and and swollen tissue from anesthetic , how accurate it can be, any tips on that .
thank you for all what you do and share
joseph
Hi Dr. Akhikar –
Those are great questions! Check out this Tuesday’s upcoming Newsletter in the Q & A section to see my responses!
Thanks –
my ques is same dr Joseph.
Also i would appreciate if u can give insight on on final prosthesis for all AOX
Hi Dr. Abbas,
Check out this Tuesday’s upcoming Newsletter in the Q & A section to see my responses regarding intra-op VDO assessment. I will also be discussing types of prosthetics and how they relate to surgery in a future article and an even more in-depth discussion in my online course (planned for release late summer/early fall 2024). Stay tuned. Thanks!
Pingback: How to Work With Our Referrals & Not Against Them - AOX Surgery