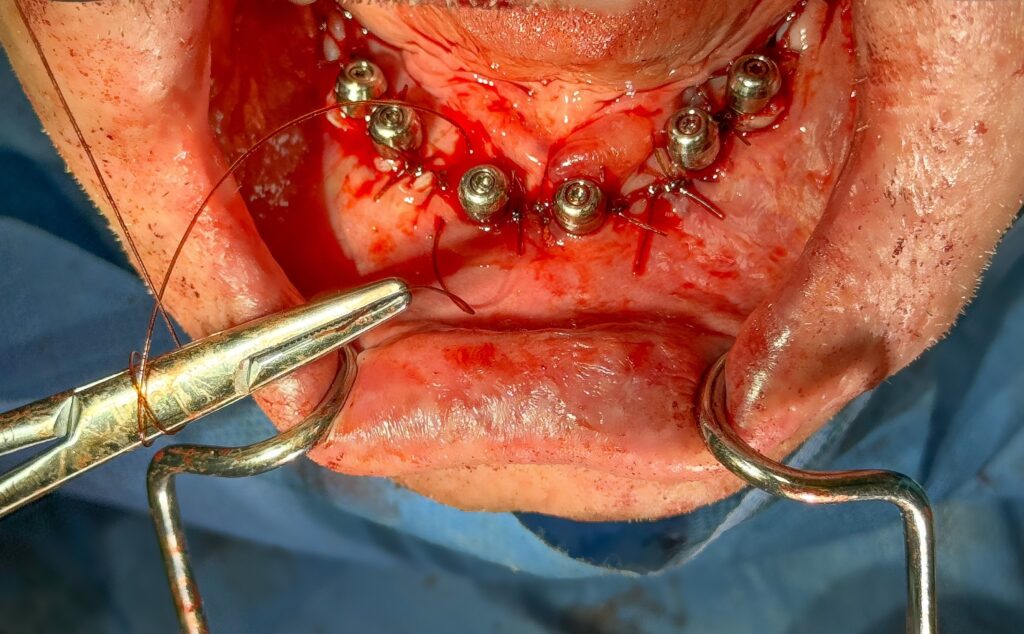
While often overlooked, I feel that closure is one of the single most important aspects of All-On-X surgery.
I believe that the quality of surgical closure directly impacts both soft and hard tissue healing.
My closure is also the most easily visible reflection of my work and attention to detail that my referring restorative providers will see.
So given the value I place on closure, what suture do I use…and why?
I use a 3.0 chromic gut suture on a C6 needle for my AOX closures.

Now I know what you’re thinking…
All this emphasis on the importance of closure and you choose to use regular old chromic gut suture?!
Let me explain a bit more…
Is this the only suture I will ever use?
There are instances where I will add an additional suture. Normally, this is if extensive bone grafting has been done.
While rare, there are times where I will perform direct sinus lifts, or other augmentation procedures, as part of an AOX surgery.
There are also times when a large particulate graft may be performed where a benign cyst or other pathologic lesion was removed.
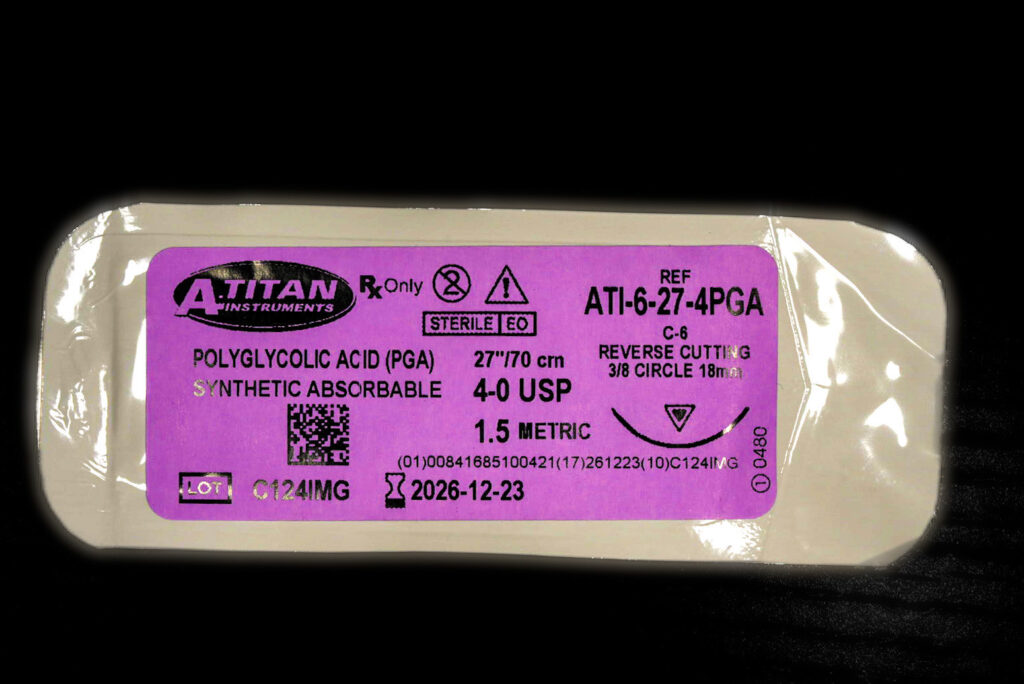
I find that both allograft and autogenous bone (though to a slightly lesser extent) create more inflammation in the soft tissue. Therefore, at these sites I prefer a longer lasting, stronger suture. In these cases I use 4.0 PGA (Polyglycolic Acid) or 4.0 Vicryl sutures.
Please note that in the grafted areas mentioned above, I will still close as I normally would with my 3.0 chromic gut suture.
However, I will ALSO go over the top of that running suture with 4.0 simple, interrupted PGA or Vicryl sutures for extra support. Because I’m going over the top of the chromic gut, I prefer the smaller diameter 4.0 suture.
So Why 3.0 Chromic Gut…with the occasional 4.0 PGA or Vicryl?
Let’s revisit the grumbling I heard earlier…
This guy prides himself on closure and he’s using regular old chromic gut suture?!
Ok, here’s the deal…
I would love to use a high caliber suture like PTFE. Monofilament sutures such as PTFE, create less soft tissue inflammation as they wick less bacteria. Therefore, they are typically viewed as better for overall soft tissue healing. The handling of these sutures is also preferred by most surgeons.
Keep in mind however, that the vast majority of my AOX cases do not incorporate any significant bone grafting or even membrane use, other than PRF.
Therefore, in the setting of routine gingival closure, I do not feel that non-resorbable monofilament sutures carry as many benefits as they would in large bone augmentation cases where there is an increase in tissue inflammation.
Furthermore, with respect to AOX surgery, there are two major issues with using a non-resorbable suture like PTFE.
1. AOX patients are immediately loaded with a prosthesis.
Access underneath the prosthetic to remove these sutures is extremely difficult. And…it is not advisable to remove the prosthetic for suture removal, prior to the 4 month healing mark.
2. Many AOX patients have a very strong phobia of the dentist.
This is a big reason that these patients have presented with a terminal dentition and why they don’t want to go back through traditional dental treatment.
Given this fact, I consciously try to limit any unnecessary surgical intervention, no matter how small, especially when my patients are awake.
I do not find it good practice to subject my patients to sitting through 2 week suture removal appointments. It would be difficult for me to work under the prosthetic and an unpleasant experience for them.
So we have established that we need something resorbable…

Given that criteria, I prefer chromic gut suture over plain gut or PGA/Vicryl suture for the following reasons:
1. I prefer the handling of chromic gut over both plain gut and PGA/Vicryl.
This is purely personal preference. Most will argue that chromic gut does not have great handling. However, I have used it sooo much over the years that I know it well and prefer its feel when closing.
Many people prefer PGA or Vicryl. I do not. You can make your own mind up…
2. I want my suture to last around 10-14 days.
I find that if it resorbs sooner than this, the wound tends to dehisce.
For this reason, wound dehiscence in my hands is more frequent with plain gut. It is too short acting.
A study by B Foment et al. found the mean longevity of chromic catgut sutures post-operatively with concomitant use of Chlorhexidine to be 11.4 days. ¹
This is exactly the time frame I am looking to achieve.
I find that if it lasts longer than this 10-14 day period, patients complain about the irritation and feeling of the sutures in their mouth.
Patients frequently express annoyance and discomfort with the longer lasting PGA or Vicryl sutures… Which can and do last weeks.
The same study mentioned above found the longevity of Vicryl sutures post-operatively with concomitant use of Chlorhexidine to be 22.7 days. ¹
This is why I only use PGA around large graft sites with more inflammation and wound tension.
Well, it’s not rocket science…but given the handling, resorbable nature, the timeframe in which it resorbs, and the absence of large graft sites in AOX surgery, I prefer and almost exclusively use 3.0 chromic gut suture to close my All-On-X incisions.
P.S.
Yes…there are new sutures being developed all the time.
And yes, there are some resorbable monofilament sutures hitting the market, that while expensive, may be good candidates for AOX surgery.
I am always open to change and using something “better”.
At this point, however, I do not feel there is enough evidence that a suture 4 or 5 times the cost of chromic gut provides an increased clinical outcome specific to AOX surgery, especially in the absence of closure over membranes or grafted sites.
In the future it is possible that I may make a change. However, at this time, for all the reasons above…I still prefer 3.0 chromic gut and I feel it performs very, very well for my patients.
It’s closing time…
Matt Krieger DMD
References:
- Fomete B, Saheeb BD, Obiadazie AC. A prospective clinical evaluation of the longevity of resorbable sutures in oral surgical procedures. Niger J Clin Pract. 2013 Jul-Sep;16(3):334-8. doi: 10.4103/1119-3077.113457. PMID: 23771456.

Curious why 3.0 and not 4.0 CG? Quicker and easier bite with the larger needle?
There is no evidence based clinical difference for closure of full arch surgery (that I am aware of) between 3.0 CG and 4.0 CG. The only reason I use 3.0 CG as opposed to 4.0, is that I just like the feel of 3.0 better. That’s it. I think 4.0 is totally fine to use in this setting and I know a handful of great AOX surgeons that prefer 4.0 CG.
do you perform continues interlocking suture or single interrupted suture , how you manage to have the tissue close nicely around the MUA
thank you
Hey Joseph! *I do have an upcoming article on “exactly” how I close and also how I make my incision – that may answer these questions in more detail.
But briefly, I run a continuous suture (typically non-interlocking) from implant to implant and then tie off. So in the maxilla, from site #1-#4 and tie. Site #4-#7 and tie. Site #7-10 and tie etc. This is more efficient than interrupted sutures but it gives me some peace of mind that if one suture comes undone – the entire arch does not dehisce – it is just one section.
The biggest part of having the tissue close nicely, is actually extracting teeth first, and the subsequent ease with which you can make your incision in a way to set up proper closure. You can read a bit more about this here.
I know you discuss soft tissue management in your Teeth First Flap Second article but maybe you could include managing thick tissue (ie palatal) before closure with the upcoming article. Maybe I just need more reps but I find trimming the palatal tissue a bit time consuming of a step for me
Hi Sean – sure I will try to incorporate this into some upcoming content. I will say that in my hands I rarely have to “thin” the palatal tissue. I will absolutely do it if necessary, but it’s honestly probably 1/100 maxillary arches where I will actually do this around abutments. I do not find the thickness of the palatal tissue to be an issue (most of the time). I typically use 2.5mm abutment heights (not sure if you are using 1.5mm?). I do, however, normally remove some excess tissue in the tuberosity region and thin the tuberosity tissue from time to time to allow for a uniform closure without the tissue bunching up in this region.
Hi doc! Do you put all the sutures youre gonna use in a metal tray filled with saline for better friction while use? Or rub the sutures with lubricant? Thank you in advance!
Hi Ziad,
I typically place the chromic gut sutures in saline about 5 minutes before I am ready to use them. When they come out of the package they have “memory” and want to fold back into the shape of the package. With a few minutes in saline, I find that they lose this “memory” and are easier to handle. It’s solely a matter of personal preference and has no real magical value other than surgeon preference.
Pingback: Exactly How I Close My All-On-X Incision - AOX Surgery