In a previous article titled Benefits of Performing Reduction on Both Jaws Prior to Implant Placement, I discussed 5 key advantages as to why I prefer to perform my bone reduction on both jaws prior to implant placement.
However, in that article I alluded to the fact that there are certain scenarios in which I do not perform this technique. In these instances, I will actually cut one jaw to completion (abutments placed and surgical sites closed primarily) before starting the second jaw.
The biggest downside to performing one jaw at a time is that it less efficient, as we are required to utilize the same instruments on two separate occasions.
That being said – efficiency is not the driving force behind how I operate. I operate first to perform the highest level of surgical quality – and then attempt to do so as efficiently as possible.
So today, I want to address 5 scenarios in which I feel it is more beneficial to actually cut one jaw at a time.
I also want to preface that, regardless of which technique is used, I always start with the upper jaw. I have discussed why in a previous AOX Newsletter.
When and Why I Will Cut One Arch at a Time
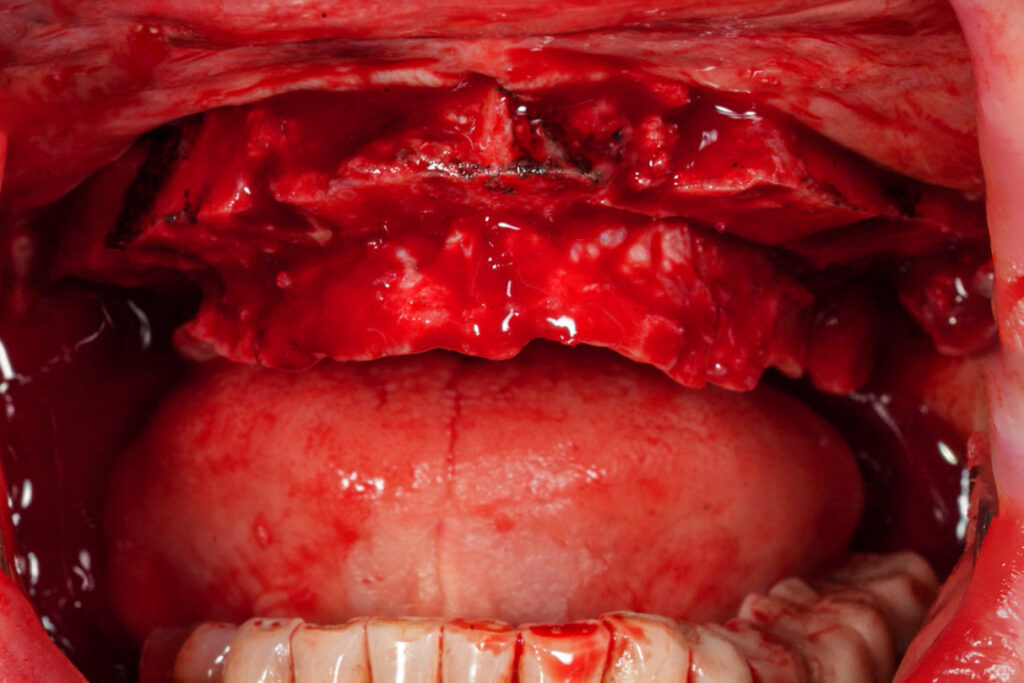
1. When I anticipate increased intra-operative bleeding.
While cutting both jaws at once is very efficient, it can also be very difficult if there is heavy bleeding. Since both flaps are open, bleeding from one jaw can obscure visualization of the surgical field while working on the opposite jaw, or at a minimum, be incredibly annoying.
Dealing with heavy bleeding while trying to cut both jaws at once can actually slow us down significantly. In this scenario, simultaneous bone reduction can therefore actually impair efficiency and increase surgical difficulty unnecessarily.
This is why I will elect to cut one jaw at a time in patients whom I suspect a likely increase in intra-operative bleeding. This allows for improved hemostasis prior to initiating the second jaw, better visualization of the surgical field, and in reality – improved efficiency.
The patients in which I anticipate increased bleeding are typically:
- Patients who are anticoagulated or on anti-platelet drugs during the peri-operative period.
- Patients with extensive periodontal disease.
- *Any patient whom I note to have increased hemorrhage during surgery. If I start on the maxilla and note more bleeding than usual – I will simply adapt my plan and perform one jaw at a time.
2. When I expect increased post-op edema or ecchymosis.
The longer our surgical flap is open, the more bleeding we will encounter and the more post-op edema our patients will have.
Therefore, if I have a patient that I suspect will experience a greater degree of bruising or swelling, I cut one arch as efficiently as possible and then close the wound as soon as possible. This limits the amount of time that the flap is open, and in turn helps reduce subsequent post-op edema and ecchymosis – at least enough to make me feel better…
Who might these patients be?
- Patients who are anticoagulated or on anti-platelet drugs during the peri-operative period.
- Patients with extensive periodontal disease.
- Elderly, frail patients with thin skin and/or a pale skin pigmentation. This type of skin will be more prone to ecchymosis. You can often see existing bruising on the arms or hands of these patients.
3. When I feel that the arch will be a very difficult surgery.
There is no medical or surgical rationale for this decision. This is purely a mental strategy that I find helps enhance my focus.
If I anticipate that an arch will be very challenging surgically, such as a severely atrophic maxilla, I typically cut that arch to completion prior to moving on to the mandible.
I want complete mental focus on the difficult arch at hand. I don’t want to be thinking about anything else – including the opposing arch.
I also want the “feel” of my osteotomies and their angulations to be fresh in my mind. This ensures I can accurately gauge my implant size selections and maintain that exact same angulation with placement, as there is typically little to no room for error.
4. When I am treating a very medically complex patient with the potential for difficult anesthesia.
Full-arch patients often present with multiple comorbidities and there can be some notably sick patients.
Once in awhile there are patients that are ok for outpatient anesthesia, but they may have a higher likelihood of having an intra-operative need that necessitates a quick finish to the surgery and/or an immediate emergence from anesthesia.
For these patients, I cut only one jaw at a time. This is so that if my CRNA were to communicate a problem to me, I could efficiently finish one arch – and then have the patient return for the second arch at a later date in order to minimize overall anesthetic time. Or, I could simply close the arch I’m on and we could have the patient addressed and optimized from a medical standpoint if necessary, prior to pursuing the remaining planned surgery.
The last thing I want in a scenario like this is to have all of the patient’s teeth out and both flaps open – and then to encounter a situation where we cannot continue that surgery as planned from an anesthetic standpoint.
Fortunately, knock on wood, this is not a situation I have encountered to date – but it is always one for which I plan.
5. And… Sometimes I’m just mentally exhausted.
There are times when I’m just tired. Whether it’s multiple surgeries in the office, life in general, or being under the weather – I just don’t have it in me to be “as efficient as possible”.
In these cases, I find I’m able to perform a more optimal surgery by simply giving my mind one thing to focus on at a time.
If I’m not “feeling it” – I do one jaw at a time to completion – and I don’t for one second feel bad about it!
While performing reduction on both jaws prior to implant placement is normally the most efficient way to perform full-arch surgery – it is not always the best.
And, while I do often perform both arches simultaneously, the 5 scenarios listed above are when I prefer to perform only one jaw at a time.
I love efficiency.
But quality is always the first aspect of surgery that goes into my decision making. I hope that this article can help you blend efficiency and quality as well in your full-arch treatment planning.
Matthew Krieger DMD

Pingback: Your AOX Questions Answered (Part 2) - AOX Surgery