Archived Newsletter Re-Post.
The AOX Newsletter • April 2024 #14
I’m a huge fan of Graphite-Guided Surgery. This technique, however, relies heavily on being able to utilize anatomical references or bony irregularities to demarcate where to apply our graphite-guide.
When delineating our implant sites on the mandible, we will always have a consistent, reproducible piece of anatomy to reference and help position our implants – the mental foramen.
However, on the maxilla, things aren’t always as straightforward. If we’re not careful, we can lose our orientation.
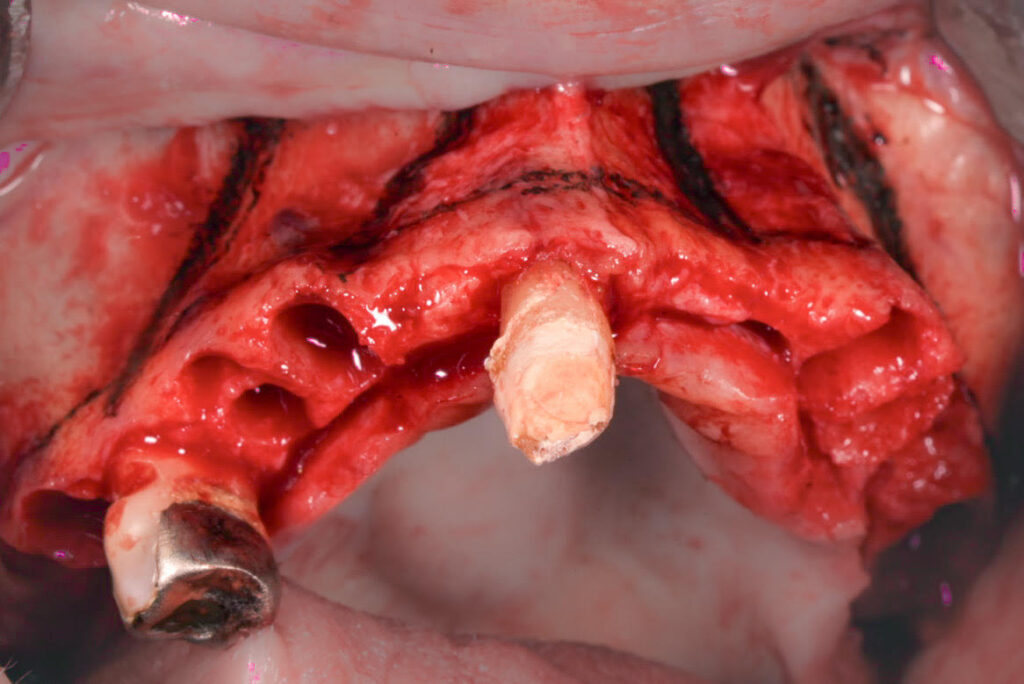
For this reason, BEFORE any bone reduction is initiated, I mark both my bone reduction line and the proposed implant locations with the sterile surgical graphite device (as shown in the photo above).
Doing this provides 3 main benefits.
1. While not common, there are times where reduction requirements (such as high smile cases) can take us below the level of some (or a handful) of the existing sockets.
The existing sockets are the easiest way to identify our osteotomy sites and reference our implant angulations. Without them, it is easy to lose our spacial awareness. In essence, we have created an “edentulous-like” scenario and are now unsure as to where to place our implants.
But, if we apply our graphite-guide while the sockets are easily visible, we know our lines are accurate – regardless of if the sockets are still visible or not after reduction.
2. On partially dentate and/or edentulous patients, I often utilize an identifiable irregularity in the bone as a guide for implant placement.
If this bony irregularity is visible on the panorex image and also appreciated clinically, I can reference it relative to my proposed osteotomy location to help guide application of the intra-operative graphite-line in this region.
This can be something such as a previous partially healed extraction socket or even a slight, but noticeable difference in bone height.
However, as you can imagine, after bone reduction these irregularities are usually no longer visible and are therefore no longer of any help to me. As such, referencing them to help apply my surgical graphite-guide is always done before reduction – when these bone irregularities are easily identifiable.
3. Finally, in an effort to maximize efficiency (while not diminishing quality), I try to pick up my surgical graphite device once and mark both the reduction line and implant sites at the same time.
This avoids picking up the sterile graphite device on two separate occasions to carry out what could have been accomplished at one time.
Here’s to simple, yet accurate.
Matthew Krieger DMD
“Success needs a process”.
Unknown
Q & A with Dr. K

“Do you ever delay an AOX surgery when there is active infection in the area?” |
Yes. I actually just did this last month.
I had a patient present to clinic for an upper/lower AOX consult with a significant right buccal space swelling.
Therefore, I saw the patient initially for extraction of 3 teeth and incision and drainage of the right buccal space abscess.
I then waited for confirmation of adequate healing, including primary soft tissue closure and resolution of all edema.
The patient was seen 4 weeks after the I&D for an immediately loaded upper/lower AOX surgery.
Archived newsletters are released on a delayed timeline, a few months after the original publication. If you would like to receive these newsletters in real time please sign up here.