Today’s post is a continuation of the most recent article titled, Your AOX Questions Answered (Part 1). This article, in similar fashion, will answer additional full-arch surgery questions that were submitted by you via a recent request on Instagram at @aoxsurgery.
Below are your questions and my responses on how I would handle the proposed surgical situations. Please keep in my mind that there are always multiple full-arch opinions. These responses simply highlight how I prefer to operate.
Your Questions:
1. Are you comfortable having exposed threads on an atrophic maxilla when using the “palatal approach”? What about on a severely atrophic mandible?
Before answering this question I want to define “palatal approach” in order to ensure that all readers are on the same page.
The palatal approach is a technique that is used in severely atrophic maxillas (think of a 1 mm or 2 mm knife-edge ridge). With this approach implants are placed “palatal” to the crest and engage the expanding palatal aspect of the ridge as the implant progresses apically. This allows you to place a narrow diameter implant in a ridge that might actually be only 1 mm wide at its crest.
This technique is one that I love and use frequently in atrophic cases. The alternative to this technique would usually be zygomatic implant placement. In my hands, I prefer the palatal approach.
I am not sure who developed this technique – but it’s referenced in the literature as far back as 1999 (See below for a few references should you desire to read more).
One theoretical downside to the palatal approach, is that by its very nature there will be palatal implant threads exposed (not fully housed in bone). This can typically be anywhere from 2-5 threads depending on the diameter of the ridge and the palatal anatomy.
With that in mind, let’s revisit the question above. Am I comfortable having exposed threads on an atrophic maxilla?
The answer is yes.
Listed below are the reasons why:
- The thick, resilient, keratinized palatal tissue seems to do an incredible job at protecting the implant body and preventing further bone loss, despite the exposed threads.
- Additionally, successful use of this technique has been shown in the literature without any grafting of the exposed threads. (Mattsson T, et al.)
- Studies have also shown similar success rates between palatally placed implants and traditional, mid-ridge placed implants. (Candel-Marti E, et al.)
- Anecdotally, I have used this technique many, many times and seen it perform surprisingly well.
The second aspect of this question asks if I am comfortable with exposed threads on mandibular implants.
The maxilla is not the only jaw that can present with severe resorption. Our friend the mandible can also present with significant knife-edge ridges and challenging anatomy. Fortunately, this seems to happen less frequently in the mandible than in its counterpart. But, it happens nonetheless.
Discussing how I handle these cases is a whole article in and of itself. However, to address the question:
I am not as comfortable with exposed threads on the mandible.
The simple answer as to why is that there is not thick palatal keratinized tissue draping over the exposed implant threads. It is most often a thin, mucosal tissue. Furthermore, in the floor of the mouth this tissue is also often “mobile” and moving around with the action of the tongue.
Does this mean that I never have exposed threads on the mandible? No, it doesn’t. There are times where I will still have exposed threads on the mandible in severely atrophic scenarios. I am just not nearly as comfortable with this situation and that is why in the atrophic mandible I employ a number of other techniques first, before considering any exposed threads.
2. Have you ever had to stop a surgery unexpectedly? What would be your advice for someone if we get into a surgery and we simply cannot place the implants?
I have not yet had to stop a surgery unexpectedly, but I do plan for this and anticipate that with enough arches this will occur at some point.
The likely reason for having to stop a surgery unexpectedly is a medical emergency.
Obviously we cannot predict when a medical emergency will occur. However, in patients that are high risk from a medical and/or anesthesia standpoint I will cut one arch at a time. In this way, if something occurs where we need to either move more efficiently to finish quickly (maybe blood pressure is notably elevated and unable to be controlled) and/or a true emergency occurs where the surgery needs to be stopped – I only have one arch to focus on. This might mean finishing this arch efficiently, or simply closing the arch and coming back after the patient is stable, or even packing the area while emergency protocols are initiated.
The point is, in higher risk patients, I actively try to avoid a scenario where I have two flaps open, bleeding from two wounds, and now am in a situation where I have to “stop” the case unexpectedly.
As a final note, if the scenario as to “why” you cannot place the implants is not medical emergency related – then it simply comes down to learning to be more adaptable and following The Cardinal Rule of AOX Surgery. Always leave yourself outs.
3. If you had to utilize guided surgery, which of the following would you choose?
- Partially-Guided (Pilot drill only)
- Fully-Guided
- Dynamic Navigation
- Computer Assisted (YOMI)
For those of you that have read my previous articles, you know that my absolute preferred full-arch guide is: Graphite-Guided Surgery.

But, if that was not an option, of the choices listed above – I would select “Dynamic Navigation”.
The reasoning for this selection is that this is essentially a very expensive graphite-guided surgery. I am getting real time feedback, without a clunky guide, and have the ability to perform immediate, on-the-fly surgical changes. I can easily adapt. This flexibility and operator control is what would appeal to me.
*As a side note, I do feel that dynamic navigation and computer assisted implant placement are the future of full-arch surgery. However, as someone who is not a true expert on this technology (from the outside looking in) I feel that improvements are still needed in the areas of efficiency and allowing for experienced provider control & adaptability – before these systems are ready for a true integration into the AOX space.
4. How do you go about presenting finances to patients?
I hate to dissapoint you with the answer to this question… but I have no choice.
I don’t, and have never, discussed full-arch finances with patients.
Having only worked as a full-arch surgeon at dedicated full-arch centers – the financial aspect has always been handled by the practice and is completely out of my hands and control. And quite frankly, that’s how I prefer it.
I focus only on the surgical aspect and do not discuss finances with patients.
I understand this is not the scenario many of you are in, but I am also not going to advise you on how to handle a situation I am not experienced at handling.
5. How far do you reflect the palatal tissue? And, how do you handle the nasopalatine nerve when reflecting the palatal tissue?
I don’t have a “set amount” that I reflect the palatal tissue. It is case dependent. That being said, I’m definitely not shy when it comes to reflecting the palate. I want this tissue out of the way so that I can adequately see the entire ridge, perform bone reduction without any tissue interference, and have room to place a malleable retractor between the tissue and bone for protection from my barrel bur.
As far as the nasopalatine nerve, I simply work around it. It will be uncovered in virtually every reflection and visualized. I don’t cut it or attempt to cauterize it etc. I just leave it be and work around it. There are times where I will have to remove bone immediately around the nerve to provide adequate reduction. In these cases I do my best to leave the nerve intact and undisturbed while working adjacent to it. No real magic here.
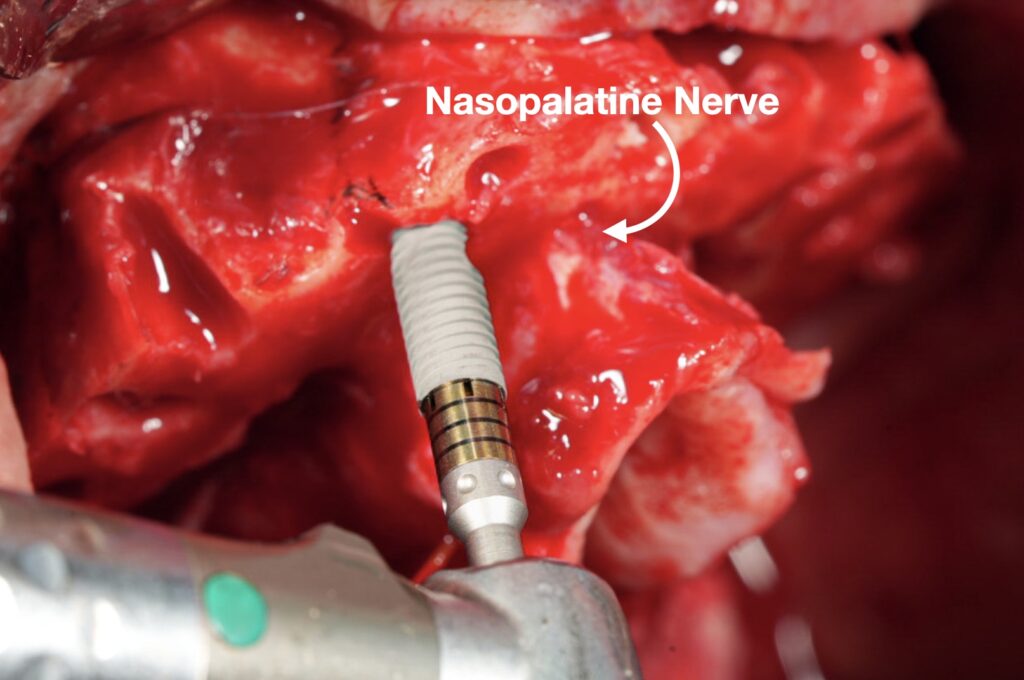
I will note that while I don’t worry too much about the nasopalatine nerve, I do exercise caution reflecting my palatal flap in the molar region, as damage to the greater palatine artery can create significant bleeding.
6. What do you think is the long-term prognosis of a full-arch prosthetic? What do you tell patients is the lifespan of a full-arch prosthetic? Patients often ask, “These last forever, right?”
Great question.
I don’t know what the long-term prognosis is for a full-arch prosthetic. I don’t know that anyone does. They have not been around long enough and studied in a large enough volume with controlled variables to accurately answer this question.
That being said, my first full arch position was at an AOX center that had been open for almost 20 years. I did see patients who had surgery 8, 12, or even 15+ years prior with full-arch implants and restorations in place and still doing well – with minimal bone loss. I have also seen patients return 4 months, 1 year, or 3 years later with failing prosthetics and detrimental bone loss.
My conclusion is this:
We know that single unit dental implants can integrate and last a very long time. While we do not know exactly how long full-arch prosthetics can last – I am confident that with a skilled surgeon and restorative provider and a compliant patient with good hygiene, full-arch prosthetics can also last a very long time.
I never set a time frame with patients. “Oh, this will last 10 years… or 20 years… or the rest of your life”. I tell patients the truth. And the truth is that we don’t really know… I prefer to say something to the effect of:
“We don’t know how long full-arch implants and prosthetics last from a large scale research based standpoint. We know that well cared for implants usually integrate with a high success rate and tend to do well over time. Many implants last for years and years. That being said, we also know that if the implants are not well cared for with an adequate home hygiene routine – just like teeth – they will likely fail in a short period of time. It is important to understand that these implants still need attention and care from an oral hygiene standpoint. Our goal is to give you a long term solution. However, there is no research based time frame that has been proven to be expected, and furthermore, this time frame will vary in each and every patient depending on a number of factors, including things like medical and health related problems, bite force and tooth grinding, and the patient’s commitment to hygiene.”
The idea that these “last forever” is a recurring assumption amongst patients. This is also true regarding the idea that since the teeth are removed, patients no longer have to do any “cleaning” and are immune to any dental problems.
The desire for a “forever prosthetic” is completely understandable. It is also, however, a humble reminder as to why patient selection is important. It is important that patients understand that we cannot “guarantee” forever. No other surgeon does this (think of orthopedic surgeons) – and neither should we. The key is in educating the patient properly.
As I’ve noted before, patient selection is important. There are patients that I can perform a full-arch surgery on – but that I do not, because I do not feel they are good “long-term” candidates. A patient that demands a prosthetic that lasts forever… probably wouldn’t qualify as a good full-arch candidate in my opinion.
Thank you to all who submitted questions! I enjoyed reading and responding to them. I hope my responses were helpful and provided at least some insight into your areas of full-arch surgical interest.
Sincerely,
Matthew Krieger DMD
References:
1. Mattsson T, Köndell PA, Gynther GW, Fredholm U, Bolin A. Implant treatment without bone grafting in severely resorbed edentulous maxillae. J Oral Maxillofac Surg. 1999;57:281–7.
2. Candel-Marti E, Peñarrocha-Oltra D, Bagán L, Peñarrocha-Diago M, Peñarrocha-Diago M. Palatal positioned implants in severely atrophic maxillae versus conventional implants to support fixed full-arch prostheses: Controlled retrospective study with 5 years of follow-up. Med Oral Patol Oral Cir Bucal. 2015 May 1;20(3):e357-64. doi: 10.4317/medoral.20262. PMID: 25662546; PMCID: PMC4464924.